What to do if parathyroid glands are removed. Adenoma of the parachitoid gland. Functions of parachitoid gland
One of the most frequent causes of hyperparathyroidism is considered the occurrence of such pathology as the adenoma of the parachitoid gland.
This neoplasm of benign nature can be capsules from 1 to 5 cm, weighing up to 85 g, which are easily separated from the endocrine fabric, which is easily diagnosed on the ultrasound.
What threatens such a state?
Small pan-shaped glands, on the back of the thyroid, as a rule, consist of 4 pieces.
Their increase is accompanied by an overabundancy of the gland hormones and as a result - leaching calcium from the bones of the skeleton. If this formation is larger than the norm, the doctors check it on malignant.
Interesting!
Very rare, with abnormal development, their number can reach 12.
In these volumetric formations, synthesis occurs, which in its action is opposite to calcitonine.
In co-action, with the involvement of the work of vitamin D, these hormones are responsible for controlling calcium exchange and phosphorus in the body.
They are responsible for the following processes:
- bone formation;
- the work of the kidneys;
- intestinal work;
- work muscles;
- work cardiovascular system.
In violation of the production of one hormone or a lack of vitamin D, irreversible consequences begin in the work of the body.
The most unpleasant disease arising from the adenoma of the parathyroidism is hyperparathyroidism.
The adenoma of the miscarriage is found in most cases in women of childbearing age and rarely in men. In children and adolescents, it does not develop.

Types of adenoma nearby
According to the results of histology, a patient may be detected by one of the following forms of parathyroid tumor:
- benign gland epithelioma;
- water-cell adenoma;
- tempelled neoplasm;
- acidophile cell adenoma;
- lipoenoma.
In the event of a particular major education, carcinoma is quite likely.
The number of cancers accounts for up to 3% of all cases of diagnosis of this pathology.
The reasons for the adenoma of Parastechidi
The main factors provoking the formation of aden on the parenchyma of the parathyroidism can be the following reasons:
- Changes in the work of genes responsible for the division of parachite cells.
- Traumatization of the cervical spine, osteochondrosis.
- Radiation therapy, whose area gets neck.
- Permanent disregard for food containing calcium.
In the diet of each person, fermented dairy products should always be located to prevent cases of hyperparathyroidism.
In some cases, it is possible to turn on the nutrition of the sesame and mushrooms of chanterelles that are saturated with the necessary trace elements.

Symptoms of the disease
The adenoma of the parathyroid gland can manifest the symptoms of the disorder of the following systems:
- Renal with complications in the form of urolithiasis.
- Bone With manifestations of severe states of osteoporosis.
- Cardiovascular, With violation of the work of Karanar.
- Gastrointestinal, with ulceal exacerbations.
At the same time, the main symptoms of the parachite gland adenoma will be the following:
- weight loss;
- weakness;
- dizziness;
- periodic pain in epigastrics;
- impairment of the enzyme system and abundant allocations of bile;
- convulsive states;
- intellect violations.
The most severe manifestation of the hyperparathyroidism in the occurrence of the paracted gland tumor becomes the development, which may end with a coma or fatal outcome due to the occurrence of internal bleeding.
If the level of calcium in serum is exceeded in more than 3.6 mmol / l, resuscitation measures for the patient's help must be carried out.

Diagnostics
Conducting diagnostic measures to identify the disease of the parachitoid gland leads to the need for consultation from specialists of the following regions of medicine:
- endocrinology;
- gastroenterology;
- cardiology;
- nephrology;
- neurology.
The main diagnostic method is screening blood and urine for the presence of the following deviations:
- Increased PTG indicators in serum.
- Increased calcium performance in the blood and when taking a daily rate of urine.
- Reducing phosphorus indicators in the blood.
- Lowering the level of vitamin D in the basic biological fluid of the body.
To conduct visual confirmation of the presence of a tumor of the thyroid gland, resort to the help of the following instrumental methods of diagnosis:
- ultrasound examination;
- thermography;
- arteries;
- x-ray x-ray;
- urography of the urogenital system;
- ECG and EGDS.
With the help of these diagnostic methods, you can set the exact nature of the destruction of the pschzch and build an effective treatment scheme.
It is carried out after careful ultrasound diagnosis of the gland and considers only the removal of the tumor of the parachitoid gland. The features of it are as follows:
- small traumatization of neck tissues (incision to 2 cm);
- fast operation of the operation (up to 10 minutes);
- the patient immediately goes home.

For this kind of operations it is necessary to have high-quality video equipment, as well as special tools.
The cost of such an operation in Moscow may be about 60 thousand rubles.
The advantages of this method can be considered:
- Minimum discomfort due to low pitfall after surgery.
- Lack of influence on voice ligaments.
- Modern materials for the seams will make them imperceptible after removing the threads.
- Application, if necessary, cosmetic seam, which will be invisible after the operation.
Such procedures are carried out on high-quality European equipment by specialists who have a high level of qualifications and interaction experience with endoscopic medical equipment.
Removal of parachitoid glands in the conditions of this method is carried out as comfortable as possible and safe for the patient.
Forecast of Life
When the adenoma of the parathyroid gland is removed, the forecast of life may be favorable if this operation was carried out at the initial stage of the disease.
At the same time, the main indicator of the positive dynamics will be considered an independent decrease in the level of calcium in the blood in the first day. Additionally, the following prevention measures are prescribed:
- regular reception of vitamin D3;
- medical massages;
- swimming.

For women in the period of Klimaks, prescribe preparations with female hormones.
Life without parathyroid glands, if applied adequate therapy with synthetic hormones is possible. With resection of cancer tumors, the forecast is less comforting.
but) History of operations on parathyroid glands. The opening of the parathyroid glands belongs to Richard Owen, which in 1850 in the London zoo found them from Indian rhino. In 1887, Ivar Sandstorm discovered them in humans. Gley, who took the work of Sandstorm, in 1890, revealed that the removal of the animals of the parachitoid glands leads to the development of Tetania.
Maccallum. In 1909, discovered the connection between the parathyroid glands and the calcium exchange. In 1907, Erdheim reported the availability of communication between osteomation and an increase in the parachitoid glands, but he explained it compensatory hypertrophy. Schlagenhaufer in 1915 suggested that an increase in the parachitoid glands is not a compensatory process, but the cause of bone diseases, he also recommended that their removal with therapeutic goal.
Only in 1925, Mandl For the first time, reported on the successful removal of hypertrophied parachitoid glands in a patient suffering from bone lesion. Shortly thereafter, several more medical centers reported a prosperous outcome of such operations.
b) Embryonic development of parachitoid glands. Little for what operations knowledge of embryology is also necessary, as for the surgery of the parachitoid glands. Understanding the principles of propagation of embryonic tissue is extremely important for predicting the normal and ectopic position of the glands. Parasitovoid glands develop from the Entoderma of the Third and Fourth Gweary Pockets.
Differentiation parachodovoid fabrics Starts at the stage of 8-10 mm of embryo. The lower parathyroid glands and thymus occur from the third gill pocket, the upper parachite glands - from the fourth. The fourth and fifth gill pocket merge, forming a caudal pharyst complex, from which the ultimobranchial vents of the lateral departments of the thyroid gland are formed. In the future, these structures move the book.
Lower parathyroid glands Timus is separated from the thymus and move to the lower pole of the thyroid gland, the upper is located at its middle third, on the side and rear. A longer path that the lower parathyroid glands goes in its embryonic development, explains the greater variability in their final location, they can be found anywhere, from the corner of the sternum before the pericardia.
IN 61% of cases Lower parathyroid glands Located near the lower pole of the thyroid gland, in 26% at the shit-thymotic bundle or at the upper border of the thymus, in 7% of cases at the level of the middle third of the thyroid gland, less often is the highest location. The upper parasite glands in 85% of cases are at the top third of the thyroid gland or slightly higher. In other cases, they tend to spread into the possession of the space, sometimes dropped up to the level of the rear-top mediastinum. In 0.7% of cases there is a location inside the tissue of the thyroid gland.
in) Hyperparathyroidism. The diagnosis of primary hyperparathyroidism is based on elevated levels of blood calcium and pararathgamon. In 80% of cases, its cause is a single adenoma, in 2-5% of cases there is a pair adenoma. The second in frequency of the cause of primary hyperparathyroidism is a parathyroid hyperplasia. In secondary hyperparathyroidism, the products of the parathgamon in one or another stumpy rises in response to hypocalcemia, most often in chronic renal failure; Treatment in most cases conservative.
Tertiary hyperparathyroidism It develops in the presence of autonomous secretion of the parathgamon against the background of a long existing secondary hyperparathyroidism.
Classic three complaints of patients with hyperparathyroidism They are considered "stones, bones and longing" caused by nephrolityiasis, fibrous osteodistrophy, osteomalacia, muscle weakness and impaired psyche. And although traditionally the development of such neuropsychiatric disorders, as depression, anxiety, a decrease in cognitive functions was associated with hyperparathyroidism, unambiguous confirmation of the improvement of symptoms after surgical correction was not received.
Currently, in most cases, the first identified patients there are no complaints. The most frequent manifestation of the disease is the presence of kidney stones. The peak of morbidity falls 50-60 years old, women are sick three times more often than men.
but - Lower parathyroid glands.Bottom parathyroid glands are located at a distance of 1 cm from the lower pole of the thyroid gland in 61% of cases
and on the shielding bundle or the upper border of the Timus in 26% of cases.
b - Upper parathyroid glands.
The upper parachitoid glands are adjacent or are upwards from the upper third of the thyroid gland in 85% of cases.
Sometimes they can descend into the possession of the space and the rear-top mediastinum.
d) Indications for operation on parathyroid glands Priv hyperparathyroidism:
I. Primary hyperparathyroidism. Indications for surgical treatment with primary hyperparathyroidism are quite clearly formulated on the basis of expert opinions, the last of which dates back to 2008:
1. Increased calcium levels in blood per mg / to above the upper limit of the norm
2. Creatinine clearance below 60 ml / min.
3. An indicator of the mineral density of tissue below -2.5 on any plot and / or pathological fracture in history
4. Age younger than 50 years
5. Pregnancy (hyperthyroidism can lead to the Age-nonsense of the parachitoid glands of the fetus)
6. Nephrolithiasis in history
7. Symptoms: Pains in the bones, neurocognitive disorders
II. Secondary hyperparathyroidism. The basis for the treatment of most patients with secondary hyperparathyroidism is the use of drugs from a group of calcium-mimetics, for example, cynakalcet. Only 0.5-1.5% of patients need surgical treatment. For those few patients whose symptoms do not improve on the background of calcium-funidic therapy, clear indications for operational intervention is not developed. General testimony for surgery:
1. Increased parathgamon level (500-800 pg / ml)
2. Heavy osteoporosis
3. High rates of bone remodeling (blood markers, scintigraphy results of bones, biopsy)
4. Hypercalcemia.
5. Increasing the parachitoid glands according to ultrasound
6. Uncontrolled hyperphosphatemia
7. Extopic calcification
8. Anemia, non-treating erythropoetin
III. Tertiary hyperparathyroidism. Most patients with secondary hyperparathyroidism are cured after kidney transplantation (thanks to the correction of causal metabolic disorders). However, in 25% of patients during the year, tertiary hyperparathyroidism develops with an increase in the level of pararathgamon.
e) Determination of the localization of parathyroid glands. The frequency of unsuccessful surgery with hyperparathyroidism can reach 5-10%. Ecctoped glands, multiple adenoma, multiple hyperplasia can cause the ineffectiveness of the operation. In order to reduce the risk of failure, preoperative research is carried out to clarify the localization of the parachitoid glands.
Justice of the Popular Council for the first time operations on parathyroid gland The patient makes it first to search for an experienced surgeon, recently questioned, especially in the light of the latest achievements in visualization and intraoperative express monitoring of the level of the parathgamon. These achievements made widely accessible methods of minimally invasive surgery of parachitoid glands.
- Technetium-99.. Study using technetium-99 is the most popular method. And the thyroid, and parachitoid glands absorb the labeled radioactive technetium. The differentiation of tissues of the glands is based on a faster removal of the drug thyroid gland. The accumulation of technetium-99 for two or three hours after administration is characteristic of parachite fabric.
It is possible to determine the location and normal, and ectopedized glands. The sensitivity of the study for a single adenoma can reach 85-100%, decreased to 37% for multiple aden. For hyperplastic glands, sensitivity is about 62%. Lower sensitivity for the hyperplastic glands compared to the adenoma is explained by the fact that the accumulation of technetium-99 occurs in mitochondria, and in the tissue of the hyperplastic glands, the content of oxiff cells is significantly less than in the adenome.
Availability multi-nobody thyroid gland It can also distort the results of the study. Surgeons should always evaluate images, especially negative, because X-ray can sometimes experience difficulties with their interpretation.
Besides preoperative diagnosticsUsing technetium-99, it is possible to determine directly during operation, whether the tumor is completely removed, without waiting for the result of the intraoperative level of the pararathgamon. James Norman with colleagues were administered to patients Technetium-99 immediately before the operation, and then with the help of gamma detectors, the level of pararathgamon was determined, synthesized by each gland.
According to " rule Norman"If the level of radioactivity in the remote iron is 20% or more of the level of radioactivity of the section of the cut or background level, then it can be considered a reliable presence of a single parathyroid adenoma, in this case the identification of other parathyroid glands is not required. According to their data, the level of radioactivity in single parathyroid adenomas is at least 18% of the background, and in most cases even higher.
While level The radioactivity of the hyperplastic glands is 16% and less. In 87% of patients, radioactivity levels in remote glands accounted for more than 20% of the background, which made it possible to immediately conclude about surgical cure.
Negative results of the study with technetium-99 are often often forced endocrinologist and a surgeon to refrain from surgical treatment. According to Norman, negative results, if the study was fully satisfied, no less useful than positive, and may indicate that parathyroid glands are usually located, i.e. Behind or near the thyroid gland.
 Ultrasound of a large parathyroid adenoma,
Ultrasound of a large parathyroid adenoma, located on the book and lateral of the thyroid gland.
- Ultrasound. The accuracy of the results of the ultrasound strongly depends on the researcher. In recent years, increasingly performed by the surgeon itself. Parasite glands are defined as homogeneous, clear formations with reduced echogenicity (compared to the thyroid gland). For adena, sensitivity and specificity is 85% and 94%, respectively, sensitivity for hyperplasia is 69%. The possibilities of visualization of ectopedized glands are extremely limited, because Those are often located in areas inaccessible to ultrasound, such as possession of the space and mediastinum.
Ultrasound can be used with a thin game aspiration biopsy. Bioptat can be sent to a cytological study, but a more sensitive method are the wasches of the parathgamon. Aspiration needle is washed with two milliliters of the physiological solution, which is sent to the laboratory to determine the level of the parathgamon. If the content of the parathgamon in the washout exceeds its serum content, then the presence of parachite fabric is considered confirmed.
- CT scan. CT is especially useful for determining the localization of ectopedized glands. The study should be carried out with thin cuts (3-5 mm) with contrast. Sensitivity and specificity with adenoma 50% and 98%, respectively, sensitivity with hyperplasia is 40%.
- Magnetic resonance imaging. MRI is also useful for determining the localization of ectopedized glands. Adenoma have a hyperintense signal in T2 mode and isointuous in T1 mode. There are 78% sensitivity reports for adenomes and 90% for ectopedized aden in the mediastincture. For hyperplastic glands, the sensitivity is 71%.
Similar emission computed tomography (Spect) and positron emission computed tomography (PET) are also offered as a means to determine the localization of the glands, but as long as they have not received such widespread as described above the technique.
- Injections methylene blue. Intravenous intraoperative introduction of diluted methylene blue stains fabric glands in a bluish color, facilitating their identification. The recommended dose is 5-7.5 mg / kg. This technique may be useful for the surgeon, even though the mechanism is not clear enough. It is necessary to refrain from the introduction of methylene blue patients receiving selective inhibitors of the reverse neural seizure of serotonin, due to the available complications of complications from the nervous system.
 Anatomical position of the upper parasites of the glands relative to returnable gangny nerves.
Anatomical position of the upper parasites of the glands relative to returnable gangny nerves. Selecting parathyroid glands follows the medial edge so as not to damage the undergoing blood vessels.
Often, parachitoid glands are identified and separated from returnable gangny nerves before the recent visualization.
In some cases, the upper parachite glands are located under the thyroid capsule, then for their separation it is necessary to work under the capsule.
e) Engineering Operations on parathyroid glands. The main stages of the revision of the parachite glands are similar to the thyroid lobectomy stages described above. We use electrophysiological monitoring of returnable hot nerves and intraoperative determination of the level of the parathgamon during all of our operations.
And although some surgeons We prefer lateral access to parachitoid glands, performing a primary cut between the front edge of the breast-curable-bed-like muscle and the lateral edge of the underprivatic muscles, we prefer medial access. It is impossible to overestimate the importance of thorough hemostasis and the need to detach the tissues along the layers of their natural location.
Bleeding during operations It makes it difficult to determine the parachitoid glands, returned gentle nerves and small vessels, blood supplying glands. The color of the glands is often described as yellowish-brown or reddish, the form of their oval. Normal iron weighs from 20 to 50 mg.
The fraction of the thyroid gland It is highlighted and shifted in the lateral direction. It is sometimes necessary to dress up the vessels of the upper pole, also to highlight the underproductive muscles and the lobes of the thyroid gland it is useful to keep the upper medial edge of the sternum-sub-surge muscle. If a preoperative examination showed the presence of an increased gland, in this place and it is worth starting its search. Otherwise begin with the place of the most typical location.
Everyone surgeon Must develop your algorithm for methodical and scrupulous search, which will allow him to find each of the four glands, regardless of whether they are typically or ectopied. After removing clearly hypertrophied glands, we solve the need to further search on the basis of an intraoperative determination of the level of pararathgamon. If the level drops by 50% and reaches normal values, the operation is completed. Otherwise, the search for the second adenoma or additional hyperplastic glands begins.
If a preoperative examination It was non-informative, we start a search from the top pole. Often it is often useful to isolate a return gangny nerve, although we do not consider it mandatory. In 85% of cases, the upper iron is located at a distance of 1 cm from the nerve inlet to the larynx, lancer and deeper. The lower iron in 61% of cases is 1 cm below and deeper the lower pole, medially returnable nerve. If there are two glands of normal size on one side, or after removal of the increased gland, the level of the parathgamon does not normate, we turn to the other side. Double adenoma occur in 2-5% of patients, in 80% of cases, the second adenoma is located on the opposite side.
If only one is found glandOr cannot find an enlarged gland, the search continues. A consistent revision of the typical location of the ectopied glands is necessary. Upper parachitoid gland can be located in descending order of occurrence: the post and side of the top pole of the thyroid gland; Pump from the larynx or esophagus; Above the upper pole of the thyroid gland. In rare cases, it can be found in the sleepy vagina or in the staircase.
With repeated looking for the bottom parathyroid gland It is worth viewing: the shield-thymotic bundle and the upper edge of the thymus, the space of the lower pole of the thyroid gland; region medially lower pole near the trachea; the lower edge of the thymus in the front mediastum; And finally, in very rare cases, the upper sections of the neck, from the lower jaw to the subyagonny bone and the bifurcation of the total carotid artery. If at this point the gland was not found, it is worth considering the possibility of terminating the operation.
Holding lobectomy On the side of the missing parathyroid glands, it is worth considering only if the preoperative examination showed the presence of parachitoid nodes in the tissue of the thyroid gland. If the glands never managed to detect, the study should repeat the research to determine their localization, including the selective fence of venous blood.
For the presence of hyperplasia in several glands Two options are possible: total parathyroidectomy with outotransplantation of parathyroid tissue at the forearm, or subtotal parathyroidectomy with the preservation of the parachitoid residue weighing 20-50 mg. Before the choice, it is worth carefully weighing the risk of transplant rejection in the first case and the possibility of recurrence of hyperparathyroidism with the need for a re-operation on the neck, which has already been audited, in the second. When preserving the remainder of the parachite gland should be marked with a clip - it will simplify the holding of re-intervention if it is necessary.
 Identification of the return gentle nerve.
Identification of the return gentle nerve.
Returnal minor nerve can be visualized or at the bottom of the thyroid artery (lower level),
or at the level of the upper parachitoid glands and Berry bundles (top level).
At a low level, a return mountain nerve can be detected within the return triangle, the boundaries of which are:
sleepy Artery lateral, trachea medial, thyroid gland from above.
To reach a returnable guttural nerve at the top level, a dull detachment in the region of the tracheopic groove with the further media share of the gland to Berry's ligament is used.
In this case, the return guttural nerve in its lower segment is not visualized. In the upper departments, the upper parachite glands are often located on recurrent nerves.
When using this technique, it should be extremely caution when separating the parathyroid glands from the tissues of the thyroid gland, trying to damage the blood vessels supplying them,
and also do not affect the return guttural nerve.
g) Key points:
The four most common forms of thyroid cancer are papillary, follicular, medullar and anaplastic.
Theodore Kohler, founder of the thyroid surgery, received the Nobel Prize in medicine and physiology for his works on the physiology of the thyroid and parachitoid glands.
The main indications of the operational treatment are cancer of the thyroid gland, suspicion of cancer, nodal goiter with severe clinical symptoms and hyperthyroidism.
According to the BETHESDA system, according to the estimation of the cytology of the thyroid gland, the Point is divided into six categories: non-informative, malignant, benign, neoplasia (follicular or the presence of Gürtle cells), suspected malignation, follicular changes in an indefinite value.
The right return of the guttural nerve is more laterally than the left.
Anomaly of the development of the Gundy Nerves is a non-returnable guttural nerve - occurs more often on the right, and in most cases it is combined with the presence of an aberrant plug-in artery (ARTERIA LUSORIA), when the right plug-in artery moves directly from the arc of the aorta and passes the stop from the esophagus.
The presence of a left non-returning nerve is often combined with dextrocardium.
To preserve the blood supply to the upper parachitoid glands, their medial edge should be carefully separated from the tisside fabric, ensuring the safety of the blood vessels of the lateral edge. Sometimes the upper parachite glands are located in a capsule or under the thyroid capsule.
The outer branch of the upper gentle nerve innervates the pisnostechoid muscle. Sometimes it passes in close proximity to the blood vessels of the top pole of the thyroid gland.
The upper parachitoid glands occur from the fourth gill pocket and are usually located next to the top of the third thyroid gland. They are located on the side and doorsually in relation to returnable gangny nerves.
The lower parachitoid glands occur from the third gill pocket and are usually located next to the lower pole of the thyroid gland. They are located medial and ventrally in relation to returnable gentle nerves.
In the case of primary hyperparathyroidism, an intraoperative decrease in the level of pararathgamon by 50% of the normal level indicates surgical cure. Radioisotopes can be used as an alternative method. Radioactivity in the remote adenoma tissue should be more than 20% of the cut level or background level. This also testifies to the success of the operation.
The task of the organ - the production of pararathgamon. In the body he is responsible for the state of nervous, muscular, as well as musculoskeletal systems, for phosphoric and calcium exchange. When the last element in the body of an excess occurs. When it is diagnosed, the removal of parachite gland is required (fully or only part of it).
Indications
The patient is assigned to the removal of parachitoid glands, when the body has the following pathological disorders:
- : Primary, secondary, tertiary.
The operation to remove the parathyroid gland is prescribed with its tumor lesion, for example, pschch adenoma or the presence of a malignant neoplasm (carcinoma).

Removal of parachite gland: preparation

In order to achieve the maximum effect from treatment, correctly select the technique and method of surgical operation, the patient passes a number of preparatory stages:
- consultation with an endocrine surgeon;
- analysis of plasma on the concentration of parathgamon, calcium;
If necessary, the MSCT is additionally performed.
In addition to the specifics, which make it possible to determine the location of pathology, as well as its nature, the patient is appointed additional preoperative diagnostics:
- expert advice (therapist, anesthesiologist, cardiologist);
- x-ray study of the chest organs;
- standard blood tests and urins.
The obtained data of additional studies helps to assess the patient's condition, readiness for the operation, and also reveal possible contraindications to the surgical operation.
Types and technology

Taking into account the fact that the size of the glands is very small, in addition to this, they are tightly in contact (they grow) with the tissues of the pin, when removing the formation, part of the parachitoid gland is excised. In particularly difficult situations, it has to delete completely.
The operation is carried out using common anesthesia. The type of drug and its dosage defines anesthesiologist, after consulting before the operation. He monitors how the patient feels during the operation.
Feature of operational intervention is to remove all pathologically changed parts of the body. Because A person has a total of 4-6 pschzh, the removal of two of them will not bring much harm and will not break the stable operation of the endocrine system and, consequently, the whole organism.
Taking into account the state of the patient and the form of existing pathology, the operation is carried out through access to the affected organ:
- Open (a small incision).
- Endoscopic (With the use of special equipment, mini-dissection is carried out).
There are several forms of operational intervention.
Open
In order to carry out an operation, on the neck (in its front), a small incision is performed. Gently, so as not to injure the muscles on the neck, the surgeon fastens the nerve (return-mountain) and the desired part in the pin.
Then excision of the modified part of the pschzh occurs.
After the procedure is completed, seam is superimposed.
Through the use of modern equipment, during the operation, it is possible to reduce damage in tissues. This contributes to the fact that after removing the parachitoid gland, the wound quickly heals and the patient is also rapidly restored after surgery performed.
Endoscopic

If there are no contraindications, a minimally invasive method is applied.
The doctor makes a small incision on the patient's neck. Through which the necessary tools and the video endoscope are introduced. Operation control is carried out using video equipment.
The picture obtained from the device is fed to the screen, it makes it possible to control the operation. Wound, which remains, is sewn with absorbing threads.
Due to this method, the patient is rapidly restored, and cosmetic defects will be minimal.
Operation is allowed even with paratyrotoxic /.
Restoration
After removing the parachitoid glands, one or part of the organ, the patient will be under control. If there is no complications, after a half months, it is allowed to return to work, and in a month - to play sports.
About what postoperative hypoparathyroidism is described in.
To prevent possible development of hypocalcemia, i.e. A shortage in the body of calcium, the patient receives certain appointments from the attending physician (special, medical preparations).
Removal of parachitoid gland: consequences
In the development of complications (swelling in operated tissues, bleeding or infection, vocal ligament paralysis), measures for intensive therapy may be required.
Parasitovoid (porous) glands - an organ that is localized on the rear surface of the thyroid. Most people have 2 pairs of them. Normally, the amount of glands can be from 2 to 8. The main function of the organ is to produce hormones affecting calcium-phosphoric exchange. In the event of tumor formations in the glands, this process is broken.
The adenoma of the parathyroid glands (paratyroenoma) is a benign hormonally active education, which is surrounded by a clearly defined capsule. Code on the ICD 10 - D34. The danger of the disease is that in the process of the growth of the tumor, squeezing the nearest tissues, which leads to their deformation and infringement of blood supply. The prognosis of the adenoma of the parachitoid gland depends on various factors: the size of education, its hormonal activity. The earlier to identify pathology and treat, the higher the likelihood of a favorable outcome.
general information

The adenoma of the parathyroid glands may be single or multiple. It is characterized by the ability to synthesize a parathyroid hormone, which leads to a critical increase in its blood level. According to statistics, 90% of primary cases are associated with the presence of adenoma.
The dimensions of education are usually small, but sometimes diagnosed paratyreaenomes about 100 g and the size of a chicken egg. More often adenoma is localized in the lower porous glands. They are surrounded by a smooth capsule, have a soft, elastic consistency. In the context of the adenoma, there has a red-brown tint, there are foci of necrosis, small hemorrhages, small-calm cavities with liquid inside.
Depending on which the types of cells form a tumor, there are several types of paratyroaden:
- alveolar;
- oxyfly;
- svetlochlochnyh;
- commonly worm.
Causes of occurrence
What is the direct cause of paratyroenomes, not fully studied. The predisposing factors of the development of pathology can be:
- genes of cells in parathyroidism;
- neck injuries;
- cervical osteochondrosis;
- the impact of radiation radiation;
- calcium deficiency in food.
Characteristic symptomatics
The clinical picture of the parasite adenoma is quite blurred, which significantly makes it difficult to diagnose.

The disease can manifest themselves with disorders of different systems:
- renal;
- cardiovascular;
- bone.
The main symptoms that should alert:
- strong sweating;
- drowsiness;
- constant fatigue;
- tachycardia;
- lowering the total tone;
- dizziness.
The adenoma of the parathyroid gland is actively producing parathgoromon. As a result, hyperparathyroidism arises for which it is characteristic:
- weakness;
- frequent vomit urge;
- constipation;
- loss of appetite;
- transmitting articular pains;
- convulsions;
- emotional breakdowns;
- depression;
- disruption of intellectual abilities.
The bone system reacts to adenoma parachidia characteristic manifestations:
- osteoporosis;
- frequent fractures and cracks of bones;
- sharing the teeth.
From the head of the gastrointestinal tract:
- strong attack of vomiting;
- frequent exacerbations of ulcerative disease;
- steatherea;
- pancreatitis.
On a note! The cardiovascular system suffers from the high calcification of the arteries, the heart valve, which leads to hypertension and can cause a heart attack. The kidney from the kidney develops nephocalcinosis, urolithiasis. All these changes are associated with hypercalcemia, which develops against the background of the elevated level of the parathgamon.
If the calcium level exceeds the mark of 3.7 mmol / l, hypercalcemic crisis can develop. It is accompanied by certain symptoms:
- pain in the opposite part;
- continuous vomiting;
- oliguria;
- gastrointestinal bleeding;
- violation of consciousness.
Diagnostics

Since the symptoms of paratyroenomes are diverse and manifests itself from different organs and systems, a comprehensive examination is necessary, consulting several narrow specialists in order to differentiate it from other pathologies.
Diagnosis of the disease includes the following studies:
- visual inspection and collection of anamnesis;
- blood test on, calcium content, phosphorus;
- subtractive scintigraphy;
- radiography of bones;
- arteriography;
- fibrogastroduodenoscopy;
A comprehensive examination makes it possible to determine the genesis of the pathology of parathyroidism, differentiate it from other diseases and properly assign treatment.
General rules and effective treatment methods
It is possible to get rid of the adenoma only by the operational way. Before conducting intervention, preparatory conservative therapy is prescribed to patients.
To suppress hypercalcemia use:
- bifosphonates;
- isotonic solution;
- Hypothiazide (thiazide diuretik);
- Sodium phosphate;
- forced diuresis.
In severe cases, it may be necessary to introduce a solution of glucose, heart glycosides, corticosteroids. The dosage of drugs the doctor determines individually, based on the age of the patient, the severity of the state concomitant pathologies. It is necessary to adhere to nutrition, which limits the use of products rich in calcium.
About the reasons and probable consequences of high levels of testosterone in women are written page.
Access to the adenome is carried out by several paths:
- open;
- reduced;
- endoscopic.
The operation is made under general anesthesia. The volume of intervention and durability can be different, depending on the specifics of the propagation of the adenoma. In most cases, under single formations, surgeons conduct organ-powered operations. In the process of their conduct, it is necessarily an inspection of all parathyroid glands and the surrounding tissues for pathological changes.
Forecast of life and recovery

If timely reveal and treat adenoma parathyroidism, then the forecast is usually favorable. Rehabilitation after the operation lasts long. During this period, it is necessary to constantly monitor the concentration of calcium to the blood. Normally, it must stabilize within 2-3 days after the removal of education.
In the launched cases, the forecast is less favorable. Long-term hypercalcemia against the background of an elevated level of pararathgamon leads to irreversible consequences from many systems. Calcium accumulates in organ tissues, in vessels, which causes appropriate changes and problems.
Paratyroadoma is good to treat. The main thing is to identify pathology at an early stage of development, and eliminate it. Otherwise, progressive hyperparathyroidism on the background of adenoma leads to severe complications. Treatment will be increasingly difficult and forecast for recovery less favorable.
Parasite glands are glands of the endocrine system, located in pairs along the rear surface of the thyroid area at the upper and lower points. In frequent cases, the violation of the function of the parathyroid glands leads to the development of hypoparathyroidism or in other words, the lack of parachite gland.
The excess of the generation of pararathgamon leads to hyperparathyroidism, in which the only treatment option is an operation. If such a need arises, and doctors recommend only the removal of parachite gland, the consequences can be very different.
With hyperparathyroidism, the production of the parathgamon increases, which leads to an increase in calcium level. To get rid of pathology applies to date, the only treatment is parathyroidectomy, in other words, the removal of parachitoid glands.
Testimony
Before carrying out the operation, the patient carefully examines the endocrinologist, and with suspected pathology, assigns the appropriate analyzes. The disease has several stages, they all require surgical intervention.
Hyperparathyroidism happens:
- primary;
- secondary;
- tertiary;
- carcinoma (malignant tumor).
The first three cases are characterized by single benign neoplasms. Multiple tumors are usually found in 2-4% of cases. Basically, they appear in secondary and tertiary hyperparathyroidism.
The situation is aggravated by chronic renal failure, against the background of which the two stages of the disease occurs. But the last case is the most serious, requires an immediate operation. Medical forecasts, unfortunately, are not always comforting.
In the photo, our readers can see where parathyroid glands are located:

Attention. Such operations are distinguished by increased complexity, so they are carried out in highly specialized medical institutions. Such clinics are equipped with modern equipment, the price of which is large enough. Preoperative qualitative diagnostics will allow for surgery with the smallest damage to healthy tissues.
Diagnostics
Operation to remove parathyroid glands is the final stage of the survey, which in several stages is conducted by the Endocrinologist.
These steps are listed in the following table:
Since both stages are very important for the treatment of hyperparathyroidism, then the instruction adopted by the international community of endocrinologists should be strictly performed.
Types of operations
Modern medicine moves forward and today there are several types of surgical interventions that are carried out on parathyroid glands.
It:
- standard operation;
- operational interference with minimal access;
- minimally invasive operation;
- video-assistant intervention procedure.
Most often use a minimally invasive operation at which the cutting of the scalpel is made no more than 2 centimeters. With this procedure, the new endovide engineer is used, which allows accuracy to determine the affected places and most correctly remove the tumor without affecting healthy fabrics.
Before the operation, biopic control is carried out, which will indicate the nature and localization of pathological changes. Also check the level of the parathgamon and calcium using the intraoperative check. After a minimally invasive operation, traces of intervention are minimal and rehabilitation period shorter than after a standard surgical procedure.

With a video intervention, special surgical objects of new generation and optical systems that help achieve the striking accuracy of the removal of affected fabrics are used. This procedure is different from other lack of pain syndrome and a good cosmetic result.
The most important stage in surgical intervention is to conduct a preoperative diagnosis. The accuracy of the diagnostic results allows you to achieve the maximum result and clearly plan the course of the operation.
Methods for removing parachitoid glands
Removal of parachitoid glands is carried out by one of two methods:
- subtotal parathyroidectomy;
- total parathyroidectomy.
Table number 1. Subtotal and total parathyroidectomy:
Important. If the patient is damaged by all parathyroid glands, radical measures are not undertaken, as it can cause nipoparatyosis. Almost three glands and part of the fourth are removed, which makes it possible to continue to ensure the normal production of the parathgamon.
Care after parathyroidectomy
The patient care after the parathyroidectomy is carried out in the hospital in the clinic, it is 2-3 days. With possible complications, the doctor can increase the duration of stay under medical supervision.
Table number 2. The rules for the patient's behavior in the postoperative period:
| Care under medical supervision | The task of medical personnel to ensure the rest of the patient in the postoperative chamber, determine the ability to speak and swallow, teach to process the seam and change the dressing. |
| Home care | Upon arrival, the patient is obliged to fulfill all the recommendations of the doctor: take calcium, check the seam for possible signs of infection, to eat only soft food during the first week, which can be easily swallowed. |
| The doctor's consultation | It should be immediately applied to your doctor if such symptoms appeared:
|
If the hazard is detected in the postoperative period, you should immediately seek advice from a specialist. Some patients have complications after surgery, which requires constant control of physicians.

Complications
In the postoperative period, some complications may arise, which no one can exclude, although such interventions rarely suggest such a risk. Surgical interventions with modern equipment reduce the likelihood of complications.
It can be:
- bleeding in the seam area;
- hoarse and loss of votes;
- reduced degree of calcium in blood;
- infection;
- difficulty in breathing and conversation;
- reaction to anesthesia;
- scarring;
- damage in nervous endings (can cause paralysis of voice ligaments).
Factors that have a great risk of developing complications in the patient:
- smoking;
- acceptance of alcoholic beverages;
- violations of the cardiovascular system.
Important. It is necessary to take into account one feature that after the operation, the patient needs to prevent the development of hypocalcemia to take the drug calcium. The instruction on the use of the drug and the term is assigned by a doctor. You also need to adhere to the right lifestyle, proper nutrition and drinking mode.
Hypoparatyosis
Separately, it is worth mentioning hypoparatyriosis accompanying the removal of parachitoid glands. This complication may be caused not only by operational intervention.
Hypoparatyroids are such:
- Postoperative (operations on the pancake glands, as well as thyroid with removal or damage to one, or several Glandulae Parathyroideae).
- Post-traumatic (caused by hemorrhage, infectious agents, radiation impacts and other factors).
- Idiopathic.
- Autoimmune.
- Congenital (due to the initial underdevelopment or lack of parachitoid glands).
Symptomatics of pathology
The leading clinical manifestation of hypoparatiraosis is the Tetanic (convulsive) syndrome, in which neuromuscular excitability is intensified against the background of a lack of separation of the parathgamon. It is manifested by strong convulsions of various muscles, which accompany pronounced pain.
Tetania precedes a number of specific symptoms:
- Numbness of skin and tingling.
- Muscle stiffness.
- The feeling of "crawling goosebumps" on the skin of the upper lip, the fingers of the upper and lower extremities.
- Cooking hands and feet.
The forerunners are replaced by convulsive contractions of symmetrically arranged muscle groups (begins with hands, then goes to the feet). In some cases, the process includes the muscles of the face, body and internal organs (depending on which of them will be affected, and the corresponding symptoms will be repaired).

The table below shows muscle groups and characteristic of them manifestations:
| Facial Syndrome Authorities | Characteristic symptoms |
| Hands | Most often the bending muscles are affected. The convulsions of the upper extremities cause them to bended in the elbow and wrist, as well as the presses of the limb to the body (a characteristic symptom of the name "Hand of the obstetrician") |
| Face | Jaws - compressed, angles of mouth - omitted, eyebrows - shifted, eyelids - half are omitted |
| Cardiac vessels | Sharp pain |
| Torchishche | The body is dispersed back |
| Neck, diaphragm, abdominal press, intercostal muscles | Bronchospasm, laryngospasm, shortness of breath, difficulty in breathing |
| Gastrointestinal tract, including esophagus | Difficulties with swallowing, intestinal colic, constipation |
| Bladder | Anuria |
| Liver | Hepatic colic |
| Kidney | Renal colic |
| Legs | The muscles-extensors are more suffering, a characteristic symptom is the "horse stop", in which the soles during the whole attack remain bent |

A convulsions with a given disease are very painful, and the frequency of their occurrence and duration depend on the form of the disease:
- When easy to develop from one to two times during the week, while the attack continues up to several minutes.
- With severe - can be repeated several times a day and last not one hour.
Cauls can develop spontaneously, but they are also able to provoke some external factors:
- Pain.
- Mechanical impact.
- Overheating or burn.
- Electric discharge.
- Loud noise.
- Hyperventilation of the lungs.

Suggesogues in some cases are accompanied by the following symptoms:
- Breathing in skin.
- Fluctuine level of blood pressure.
- Tachycardia.
- Vomit.
- Diarrhea.
- Loss of consciousness (severe cases).
Vegetative symptoms for hypoparathyroidism is very extensive:
- Strengthening sweating.
- Dizziness.
- Short-term loss of consciousness in the form of fainting.
- The feelings of "concluding" ears, the stall.
- Falling hearing.
- Concentration disorders.
- Reducing the severity of twilight.
- Arrhythmia.
- Bolt pain.
- The sensitivity disorders of various receptors (temperature - the patient throws it into the cold, then in the heat, taste - the patient perceives the acidic taste worse, but it feels bitter and sweet, the auditory - a person becomes more sensitive to the noise level, thunder and sharp sounds).

If in the peripheral blood of people suffering from hypoparatiraosis for a long time, the low content of Ca2 + ions is preserved, then changes in mental status may begin, which consist in the following manifestations:
- Falling the level of intelligence.
- Worsening memory.
- Neurosis.
- Various variants of emotional lability (buses of longing and depression).
- Sleep disorders.
Also, chronic hypoparathyroidism causes a number of tissue trophic violations:
- The skin is dry, it begins to peel and changes its pigmentation, later joined vesicles, having serous contents, eczema, fungal lesions.
- Nails - brittle.
- The hair is very early, their growth is broken, partial or full baldness gradually appears.
- Teeth fabrics are damaged, both in children (violation of their formation, in some sections of the enamel of its hypoplace) and in adults (carious phenomena is damaged and develop).
- Loge in growth in children.
- The development of cataracts, in which the crystal is muttered, which causes a drop in visual acuity up to full blindness.
- Calcification of brain fabrics.

If hypoparatyosis proceeds latently, then convulsive manifestations can occur against the background of acute infectious diseases, intoxication, hypovitaminosis, pregnancy. In order to prevent all these heavy disorders developing when parathyroid glands are lost after removal of the thyroid gland or surgical interventions on them themselves, it is necessary to start replacement therapy in a timely manner and undergo it throughout the entire periodic term.
On the video in this article, experts will tell our readers, which modern technologies and equipment are used to conduct operations to remove parachitoid glands.
 What is a hot water supply of an apartment building
What is a hot water supply of an apartment building Water supply of an apartment building
Water supply of an apartment building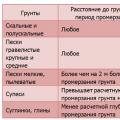 Calculation of the Load for the foundation Installed Electrical Instruments
Calculation of the Load for the foundation Installed Electrical Instruments