Active and inactive form of tuberculosis. What is dangerous hidden form of tuberculosis. What is latent tuberculosis infection
- Pathology at which the spread of the virus occurs in most cases, when coughing.
If mycobacteria is hit in pulmonary fabric, cell destruction begins, with the formation of deep cavities.
Without timely treatment, the patient with active tuberculosis can perish.
![]() Therapist: Azalea Solntsev ✓ Article verified by the doctor
Therapist: Azalea Solntsev ✓ Article verified by the doctor
Active tuberculosis is a condition in which the body's immune system is unable to deal with tuberculosis bacteria, therefore bacterial excretion develops into an external or internal environment. Microorganisms spread through air and usually affect the lungs, although they can involve other organs and parts of the body into the pathological process.
If the body resistance is low, for example, due to aging, malnutrition, infections, such as HIV, or for other reasons, bacteria are activated and cause the open form of tuberculosis.

According to estimates of the World Health Organization, every year 8 million people develop an active species of illness and almost two of them dying. Each tenth, infected with pathogenic microorganisms, can occur open tuberculosis. The risk of development is most large in the first year after infection, but the form is often developing many years later.
Immediately infected with an open form of the disease, because it is necessary to go through its first phase. When microbes of tuberculosis fall into the body, they are inactive.
Sleeping microbes do not damage the organism or do not cause symptoms of the disease. This is called latent tuberculosis infection.
It can last for a short time or many years. When the microbes are activated, the organism begin to grow and damage, then specific signs of pathology appear. This is called active or open tuberculosis.
Www.tuberculosis.emedtv.com.
Www.health.state.mn.us.
The main symptoms of pathology
The manifestations of active tuberculosis depend on the individual characteristics of the body.
The open form of tuberculosis can cause symptoms such as:
- productive cough, which lasts 3 weeks or longer;
- pain in the chest;
- isolation of sputum with blood impurities.
Non-specific features may include:
- weakness or fatigue;
- weight loss;
- anorexia;
- chills;
- fever;
- night sweating.
These possible symptoms of tuberculosis are not reliable signs of the disease. Other health problems can also cause these signs. Anyone with the likely manifestations of the illness should consult a doctor as soon as possible that the problem can be diagnosed in a timely manner and treat.
Www.tuberculosis.emedtv.com.
The risk of infection - how to get the pathology
How can I get an open form of tuberculosis? Anyone can get infected with a dangerous disorder. When someone suffering from the tuberculosis of the lungs, coughs, sneezes or talks, microbes are able to spray in the air. People are nearby, can inhale agents. It is impossible to infect the disease from a handshake or food, dishes, bed linen and other items. More others are subject to infection people with a weak immune system.
How can I get infected:
- abusing alcohol or drugs;
- having diabetes;
- in silicose;
- having cancer head or neck;
- in the presence of leukemia or Hodgkin's disease;
- in the diagnosis of severe kidney disease;
- having low body weight;
- during some types of treatment (for example, corticosteroids or organ transplantation);
- during the period of specialized therapy of rheumatoid arthritis or Crohn's disease.
If pathogens are in the lungs, you must be careful to protect other people from microbes, since the risk of infection with the open form of tuberculosis increases several times. Ask a doctor or nurse, they will tell you what to do to prevent the transfer of microbes to close and relatives and how to get infected yourself.
Www.tuberculosis.emedtv.com.
Www.health.state.mn.us.
How many live with this disease
Pathology does not always lead to death. Without treatment, life expectancy can range from 5 to 30 years, how many lives with an open form of tuberculosis depends on the set of external and internal factors.
First of all, the immune stability of the body, as well as the age and the presence of concomitant diseases.

You can expect to save your work, stay with your family and lead a normal life if sick with tuberculosis. Nevertheless, must regularly take the medicine to be confident in positive dynamics and prevent infection of other people.
After therapy, the chance for full recovery is very high, but not guaranteed 100%. There are particularly severe forms of disorders that are practically not susceptible to most antibacterial drugs.
Therefore, the importance of compliance with the prescribed impact mode cannot be underestimated. Without treatment, the disease will progress and can lead to disabilities and even a fatal outcome.
A bad forecast for life and high risk creates smoking more than 20 cigarettes per day. This increases the chance of the occurrence of pathology and hazardous complications in two or four times. Diabetes also worsens the forecasts of the ailment.
Other painful states that reduce the chances of recovery:
- alcoholism;
- the final stage of kidney diseases;
- malnutrition;
- hodgkin's lymphoma;
- chronic lung diseases.
Www.emedicinehealth.com.
Www.news-medical.net.
Open and closed form - comparison
Persons with a latent form of infection do not hurt and have no symptoms. They are infected with M. tuberculosis mycobacteria (Koch stick), but do not show signs of the disease.
The only confirmation is a positive reaction to a tuberculin skin test or blood test for tuberculosis. Persons with latent form are not indifferent for others.
In general, without treatment, 5-10% of infected people develop an open form of illness in a certain period of life. Half of them, it will happen during the first two years after infection.
In persons whose immune system are weak, especially in HIV-infected, the risk of developing an active form of illness is significantly higher than in patients with normal protection of the body.
A person with a hidden tuberculosis infection:
- typically, the skin test or the result of blood test results indicate an infection;
- normal chest x-ray and negative sputum test;
- tuberculosis bacteria in the body are alive, but inactive;
- no symptoms;
- microorganisms do not apply to others.
In some people, bacteria overcome the protection of the immune system and begin to multiply, which leads to progression from closed to the open form of pathology. Some fall shortly after infection, while others later, when their body's reaction becomes weak.
People are considered contagious for the surrounding society. In suspected, patients should be sent to a complete medical check.
The open form of tuberculosis is a very serious illness and can lead to death, without treatment. The closed form is always dangerous in that a person cannot in time to proceed to drug therapy in a timely manner.
At an infected person with an open form:
- positive skin test or blood test result indicating infection;
- anomalous X-ray of the chest or a positive wet smear, and the culture is also sewn;
- there are active tuberculous bacteria in the body;
- numerous symptoms appear, such as cough for 3 weeks or longer, hemoptia, breast pain, inexplicable weight loss and appetite, night sweats, fever, fatigue and chills;
- the spread of bacteria to others may occur;
- treatment is mandatory.
The first signs of the disease
Tuberculosis manifestations are usually developing slowly, for several months and years, often disguised by other states. Bacteria multiply very slowly, so the symptoms of the disease also appear slowly, usually from several months to many years. Many symptoms are vague and may have other reasons.
Classical manifestations of active tuberculosis are:
- malaise;
- night sweats;
- generalized pain in the body;
- periodic fever;
- weight loss and appetite;
- fatigue.
From specific symptoms - the first signs of the open form of tuberculosis is a permanent cough, which in the morning can be with yellow or green wet. Over time, traces of blood appear, although its large number is unusual.
Cough is often considered to be connected with smoking, asthma or recent disease, but forget about tuberculosis. Pathology causes the strengthening of the night trembling, while the person wakes up, impregnated later.
As the disease progressing, fatigue and indisposition increase, the weight loss and appetite progresses. Other common early phenomena are pain in the chest and shortness of breath. They may occur as a result of the formation of pleural effusion - the accumulation of fluid between thin membranes, which cover the lungs and the inner part of the pectoral wall.
Www.everydayhealth.com.
Tuberculosis and incubation period
Microbacteria Mycobacterium tuberculosis has an incredibly low infectious dose - less than 10 microorganisms to initiate the disease. Bacteria have a long incubation period: from two to twelve weeks with a range of fourteen days to several decades.
They have the ability, both to hiddenness and to initiating the active form of the disease. Mycobacteria, inhaled by the owner, infect the lungs, and is absorbed by Alveol macrophages. After that, they can remain inactive or begin to multiply within the specified cells, which causes an open infection.
The duration of tuberculosis incubation varies depending on individual risk factors.
According to data, within six weeks after infection, an infected person develops primary infection in the lungs, which has no symptoms.
Then the disorder goes into an inactive phase that can last from several weeks to several years. The incubation period can be protracted. Therefore, the risk of becoming infected with everyone who comes into contact with potentially infected.
Www.microbewiki.kenyon.edu.
Www.healthylIVing.Azcentral.com
How to protect yourself from the open form of tuberculosis
Vaccination can help protect against disease. The infectious disease is sufficient among children. BCG is provided to all babies in countries where the disease is common.
In such states as the United Kingdom, it is recommended to those who are at high risk. Before vaccination, man gives a skin test Mantu to identify the presence of hidden tuberculosis. The infection is considered the most dangerous for babies.
Prevention consists of two main stages:
- prevent people with an active phase in places of cluster of people;
- preventing the development of the active phase in people with hidden tuberculosis.
How to protect yourself at home:
- Houses must be fairly ventilated.
- Anyone who coughs is obliged to learn the respiratory etiquette, respiratory hygiene and adhere to the studied practice.
- With the positive results of the smear, patients with tuberculosis should:
- conduct as much time in the fresh air;
- sleep separately from other family members, in a well-ventilated room;
- as many time as possible is in public transport and in places where a large number of people are going.
Treatment of patients with a closed form of the disease is the most efficient method of protection against an open form of illness.
Many people with latent infection never develop an active disease.
A special increase in risk is:
- people with HIV infection;
- persons who have become infected over the past 2 years;
- babies and small children;
- drug addicts;
- elderly.
If you have a hidden infection, you need to take medicine.
Instruction
On the organization of dispensary observation and accounting of contingents of anti-tuberculosis institutions
Groups of dispensary observation and accounting of adult contingents of anti-tuberculosis institutions
Zero Group - (0)
In the zero group, there are persons with the unspecified activity of the tuberculosis process and in need of differential diagnosis in order to establish a diagnosis of tuberculosis of any localization. Persons who need to clarify the activity of tuberculosis changes include in a zero-and subgroup (0 A). Persons, for differential diagnosis of tuberculosis and other diseases, are credited in the zero-b subgroup (0-b).
First Group - (I)
In the first group-based patients with active forms of tuberculosis of any localization. Select 2 subgroups:
first-a (i-a) - patients with first identified disease;
first-b (i-b) - With the recurrence of tuberculosis.
In both of the subgroups, patients with bacterial idle (I-A-MBT +, I-B-MBT +) are isolated and without bacteria (I-A-MBT, I-B-MBT-).
Additionally isolated patients ( subgroup I-in) who interrupted treatment or were not examined at the end of the course of treatment (the result of their treatment is unknown).
Second group - (II)
In the second group, observed patients with active forms of tuberculosis of any localization with the chronic course of the disease. It includes two subgroups:
second-A (II-A) - patients who, as a result of intensive treatment, a clinical cure may be reached;
second-b (II-b) - Patients with a far-sighted process, the seraction of which cannot be achieved by any methods and which need to be associated, symptomatic treatment and periodic (if indications) of anti-tuberculosis therapy.
The patient is translated (enrollled) in II-A or II-B subgroups based on the conclusion of the CVCC (KEK), taking into account the individual characteristics of the flow of the tuberculosis process and the state of the patient.
Arrivals of patients with active tuberculosis include in the corresponding state a group of dispensary observation.
Third Group - (III)
In the third group (control) take into account persons cured of tuberculosis of any localizations with large and small residual changes or without residual changes.
In the framework of the I, II and III groups of dispensary observation and accounting, the patients with tuberculosis of the respiratory organs (Tod) and tuberculosis of the localization of localization (TVL)
Fourth Group - (IV)
In the fourth group, take into account persons in contact with the sources of tuberculosis infection. It is divided into two subgroups:
fourth-A (IV-A) - for persons consisting in domestic and industrial contact with the source of infection;
fourth-b (IV-b) - For persons who have professional contact with the source of infection.
Some questions Tactics Dispensary Observation and Accounting
Determination of the activity of the tuberculosis process
Tuberculosis of dubious activity
This concept is denoted by tuberculosis changes in the lungs and other organs whose activity seems to be unclear. To clarify the activity of the tuberculosis process, a 0-A subgroup of dispensary observation was allocated, the purpose of which consists in carrying out a complex of diagnostic measures.
Persons consisting in the III and IV groups, which have the need to determine the activity of the available changes, are not transferred to the "0" group. All questions are solved by examining and observing in the same accounting group.
The main complex of diagnostic measures is carried out within 2-3 weeks. If you need test therapy, the diagnostic period should not exceed 3 months.
From the zero group, patients can be translated into the first or directed to therapeutic and preventive institutions of the shared network.
Active tuberculosis
A specific inflammatory process caused by mycobacterium tuberculosis (MBT) and determined by a complex of clinical, laboratory and radial (radiological) features.
Patients with an active form of tuberculosis need to conduct therapeutic, diagnostic, anti-epidemic, rehabilitation and social events.
All patients with active tuberculosis identified for the first time or with recurrent tuberculosis are credited only in the group of dispensary observation. Taking them into account in the II group is not allowed.
If, with surgery in the patient consisting in the third group, signs of an active tuberculosis process were found, it is left in the third group and carry out anti-tuberculous therapy with a duration of up to 6 months.
The question of taking accounting for the first time identified by patients with tuberculosis and the removal of CEK (KEK) on the representation of a phthisiart or other specialist of the anti-tuberculous institution (tuberculosis compartment) decides. About taking under the dispensary observation and the cessation of observation, the anti-tuberculosis institution announces the patient in writing (Appendix No. 1 and 2). Notification dates are registered in a special journal.
Clinical cure
The disappearance of all signs of an active tuberculous process as a result of the main course of integrated treatment.
The statement of clinical cure tuberculosis and the moment of completion of an effective course of complex treatment are determined by the lack of positive dynamics of the signs of the tuberculosis process within 2-3 months. The observation period in the I group should not exceed 24 months, including 6 months after effective surgical intervention. From the I group of the patient can be translated into III or II group.
Bacteridians
Patients with an active form of tuberculosis, in which in the biological fluid of the organism and / or pathological material were found in the biological fluid and / or pathological material. From patients with extrapulic forms of tuberculosis to bacteria sedresses, individuals in which MBT is found in the separated fistula, in the urine, menstrual blood or discharge of other organs. Patients in whom MBT are allocated during the crossing of puncture, biopsy or operational material, as bacteries are not taken into account.
Multiple drug stability MBT is their resistance to the action of isoniazide and rifampicin at the same time, with or without resistance to any other anti-tuberculosis drugs.
Polyzerism - This is the stability of MBT to any two or more anti-tuberculosis drugs without simultaneous resistance to isoniazid and rifampicin.
In the presence of clinical and x-ray data on the activity of the patient's tuberculosis process, they take into account as a bacteriatery even with a one-time detection of MBT. In the absence of clinical and radiological signs of an active tuberculous process for taking a patient as a bacteritor, you need two-time detection of MBT by any method of microbiological research. In this case, the source of the bacterial excretion may be an endobronchite, a breakthrough of the caseous lymph node into the lumen of the bronchus or the decay of a small focus, difficult to determine the X-ray method, etc.
One-time detection of MBT in contingents of the group III in the absence of clinical and radiological symptoms confirming the tuberculosis reactivation requires the use of in-depth clinical, radiation, laboratory and instrumental examination methods in order to establish a source of bacteria and the presence or absence of active tuberculosis.
In order to establish the bacterial excavation from each patient with tuberculosis before the start of treatment, the sputum (washing waters of the bronchi) and another pathological separated by bacterioscopy and sowing should be carefully studied. The examination is repeated in the process of treatment monthly before the disappearance of MBT, which subsequently must be confirmed by no less than two consecutive studies (bacterioscopic + culture) with intervals in 2-3 months.
Epidemic focus (synonym "The hearth of infectious disease") is the location of the source of infection and its surrounding territory, within which the disseminate of the infection is possible. Communicative with the source of infection is considered persons from contact with the bacteria. The epidemic center is taken into account at the place of the actual residence of the patient. Anti-tuberculosis institutions (branches, cabinets) are a hearth tuberculosis infection. On this basis, employees of anti-tuberculosis institutions are attributed to persons in contact with bacteriamen, and are recorded in the fourth group of dispensary observation.
Destructive tuberculosis
The active form of the tuberculosis process with the presence of the decomposition of the tissue, determined by the complex of radiation research methods.
The main method of identifying destructive changes in organs and tissues is a radiation study (X-ray - overview radiographs, tomograms). With the tuberculosis of urinary organs, an ultrasound study is of great importance. With an active tuberculous process, radiological studies are carried out at least 1 time in 2 months (in I-A, I-B and II-A subgroups) to clinical cure, in the II-B subgroup - according to the testimony. The closure (healing) of the collapse cavity is considered to be its disappearance, confirmed by methods of radiation diagnosis.
Recurd
The appearance of signs of active tuberculosis in persons previously undermining tuberculosis and cured from it, observed in the group III or discontinued due to recovery.
The appearance of signs of active tuberculosis in spontaneously recovered persons who have not previously registered anti-tuberculosis institutions are regarded as a new disease.
Disaggming factors
Factors contributing to the decrease in immunity to tuberculosis infection, weighting of the flow of tuberculosis and deceleration of cure:
- medical (various non-tuberculosis diseases and pathological conditions);
- social (income below the subsistence minimum, increased production load, stress);
- Professional (permanent contact with sources of tuberculosis infection).
Gaggazing factors are taken into account when observing patients in accounting groups, in determining the timing of treatment and conducting preventive measures.
Diagnosis wording
When taking into account the detected patient with active tuberculosis (I group), the diagnosis is formulated in the following sequence: the clinical form of tuberculosis, localization, phase, bactering.
For example:
· Infiltrative tuberculosis of the upper share of the right lung (S1, S2) in the decay phase and the sector, MBT +.
· Tuberculous spondelite of the thoracic spine with the destruction of the bodies of the vertebrae of TH 8-9, IBT.
· Cavernous tuberculosis of the right kidney, MBT +.
When translating the patient in the II group (patients with the chronic flow of tuberculosis) indicate the clinical shape of tuberculosis, which takes place at the moment.
Example. While taking into account the infiltrate form of tuberculosis. With an unfavorable course of the disease, fibrous-cavernous pulmonary tuberculosis was formed (or a large tuberculus with a decay of or without decay) was formed. In the translated epicrise, a diagnosis of fibrous-cavernous tuberculosis of light (or tuberculle) should be specified.
When transferring the patient to the control group of accounting (III), the diagnosis is formulated according to the following principle: the clinical cure of a form or another form of tuberculosis (exhibit the most severe diagnosis for the period of the disease) with the presence of residual post-carcular changes (large, small) in the form (specify the nature and prevalence of changes , the nature of residual changes).
Examples:
· Clinical cosage of focal pulmonary tuberculosis with the presence of small residual posttuberculosis changes in the form of single small, dense foci and limited fibrosis in the upper part of the left lung.
· Clinical cure disseminated pulmonary tuberculosis with the presence of large residual posttuberculosis changes in the form of numerous dense small foci and common fibrosis in the upper pieces of the lungs.
· Clinical cure of pulmonary tuberculus with the presence of large residual changes in the form of scars and pleural thickening after a small resection (S1, S2) of the right lung.
In patients with extrapulmonary tuberculosis, diagnoses are formulated by the same principle.
· Clinical cake of tuberculous coxit on the right with a partial disruption of the joint function.
· Clinical cure of tuberculosis drive left with outcome in ankylosis.
· Clinical cure of tuberculous drive to the right with residual changes after surgery - the ankylosis of the joint.
· Clinical cure of the cavernous tuberculosis of the right kidney.
The procedure for dispensary observation and taking into account adult patients is presented in Table 1.
Table 1
The procedure for dispensary observation and accounting of contingents of adults registered
Anti-tuberculosis institutions
| Group / Subgroup accounting | Medical and Diagnostic and Preventive Events | Dispensary Observation Efficiency Criteria | |||
| Zero group | |||||
| 0-A. | Persons who need to determine the activity of the tuberculosis process. | Not more than 3 months. | A complex of diagnostic methods, according to testimony - trial chemotherapy. | Defense diagnosis. | |
| 0-B. | Persons who need differential diagnostic measures. | Determined by the diagnostic technique. | 2-3 weeks | A set of diagnostic events | Defense diagnosis. |
| I-A. | I-A (MBT +) for the first time identified patients with bactering I-A (MBT-) for the first time identified patients without bacteria | With outpatient treatment - daily, with an intermittent treatment - 3 times a week, in exceptional cases - 1 time in 7-10 days. | Determined by the duration of the main course of treatment, but not more than 24 months from the date of registration | The main course of treatment, in the presence of testimony - surgical treatment, sanatorium treatment. Events on social and labor rehabilitation. Sanitary and recreation and preventive measures in the foci of infection. | Achieving clinical cure and translation into the III group of accounting 85% of patients after an effective main course of treatment, but no later than 24 months from the date of taking into account. Transfer of patients in group II - no more than 10% of the number I group. |
| I-B. | I-b (MBT +) patients with recurrence with bacteria I-B (MBT-) patients with recurrence without bacteria | ||||
| I-B. | Patients who are self-respecting the treatment and outlined from the survey. | - | Transfer of patients to the I-in group is produced 1 month after the loss of contact. Stay - before the resumption of treatment or obtain reliable information about the fate of the patient (death, translation, departure). | Individual work with patients. If necessary, the organization of compulsory surveys and treatment under Article 10 of the Federal Law. | The number of patients in the I-B subgroup should not exceed 5% of the number of the entire first group! |
| II-A. | Patients, intensive treatment of which can lead to curable tuberculosis. | Individualized complex chemotherapy taking into account the medicinal sensitivity of MBT, surgical and sanatorium treatment, additional wellness activities that increase the effectiveness of treatment. Preventive events in a focus of tuberculosis infection | Achieving clinical cure tuberculosis annually in 15% of patients after transferring to the II-A subgroup. | ||
| II-B. | Patients in need of soiling, symptomatic treatment and in the event of indications - in anti-tuberculosis therapy | Determined by the state of the patient and the treatment | The duration of observation is not limited | Medical measures extending life. Surgical and sanatorium treatment - according to the testimony. Preventive events in a focus of tuberculosis infection | Increasing the life expectancy of patients, reducing the spread of tuberculosis infection by anti-epidemic and preventive work in the focus. |
| Third Group (Healing Patients) | |||||
| III | Persons with inactive tuberculosis process after clinical cure | No less often 1 time in 6 months. During the period of anticorcidal courses of treatment - depending on the methods of their conduct. | Persons with large, or small residual changes in the presence of aggressive factors - 3 years of faces with small residual changes without gagging factors - 2 years. Persons without residual changes - 1 year. | A comprehensive examination of patients at least 1 time in 6 months (according to indications - more often). Conducting anti-infertion courses of chemotherapy according to indications. When the operation of active tuberculous changes in the organs is detected in the process - carrying out combined chemotherapy to a duration of up to 6 months by testimony. Sanatorium and clotting treatment. Events on socio-labor rehabilitation. | With clinical well-being - deregistration and translation under observation of the polyclinic of the general medical network at the place of residence, followed by medical examinations 2 times a year for 3 years after removal from the accounting. Recurrent tuberculosis - no more than 0.5% of the average annual number of persons observed in the group III in the reporting year. |
| Fourth Group (Contacts) | |||||
| IV-A. | Persons consisting in domestic (related, apartment) and industrial contact with a patient an active form of tuberculosis with an established or unidentified bacterial release. | 1 time in 6 months. When contacting the bacteritor and 1 time per year, with contact with the patient, the active form of tuberculosis without installed bacteria. | The duration of the observation is determined by the cure time of the patient plus 1 year after the cessation of contact with the bacteria | Comprehensive examination 2 times a year. In the first year after identifying the source of infection according to the indications, the course of chemoprophylaxis is carried out for 3-6 months. According to the testimony, the re-course of chemoprophylaxis is also carried out, generalifying activities that contribute to improving immunity, including sanatorium treatment. Anti-epidemic events in the hearth. | The total incidence of contact persons in bacillary foci is not more than 0.25% of the average annual |
| IV-B. | Persons who have professional contact with the source of infection: employees of anti-tuberculous (tuberculosis) institutions, workers of disadvantaged in relation to the tuberculosis of livestock and birds of farms and persons who have constant contact with the source of infection. | No less often 1 time in 6 months. | Determined by the working life in professional contact plus 1 year after its termination. | Comprehensive examination 2 times a year: the first time - the radiograph of the organs of the chest, blood tests and urine, in women - the examination of the gynecologist; The second time is an inspection of a doctor-dispensarizer; Laboratory, radial, instrumental studies - according to indications. Control of safety regulations. Annually a coherent treatment rate. Chemoprophylaxis - by testimony. | The incidence of tuberculosis of persons from professional contact is not more than 0.25% of the average annual number. |
table 2
Scheme of examination of adult patients consisting on dispensary accounting
| Group / Subgroup accounting | Radiation research methods | Research of bacteries |
| 0 (zero) | Radiographs, tomograms, ultrasound (with the tuberculosis of urinary organs) before enrollment in the group, in the future at least 1 time per month (according to indications - more often). | Bacterioscopy (simple, luminescent), sowing before enrolling in the group, in the future monthly. |
| I-A, I-B, II-A | Patients with tuberculosis of respiratory organs during the course of chemotherapy: - in the intensive phase - at least 1 time in 2 months; - before the transition to the transition to the continuation phase; - in the continuation phase - according to the testimony. - before the completion of the course of treatment; Upon completion of the course of chemotherapy - according to the testimony, but at least 1 time in 6 months. Patients with extrapulmonary tuberculosis | During the course of chemotherapy: - in the intensive phase - at least 1 time per month.; - before the transition to the transition to the continuation phase; - in the continuation phase - at the end of her second month and later according to the testimony; - Before completing the course of treatment. Upon completion of the course of chemotherapy - according to the testimony, but at least 1 time in 6 months. |
| II-B. | According to the testimony, but at least 1 time in 6 months | According to the testimony, but at least 1 time in 6 months |
| III, IV. | Radiographs before enrollment in the accounting group (tomograms - by testimony). Later - at least 1 time in 6 months, according to the indications more often | The study of sputum, urine or other diagnostic material) before enrollment in the group. Later - at least 1 time in 6 months, according to the indications more often |
Notes:
1. Blood tests, urine and other laboratory studies (according to indications) produce patients 0 groups and patients with I-A, I-B and II-A subgroups in the intensive phase of chemotherapy at least 1 time per month, in the continuation phase - no less than 1 3 months times; Patients II-B subgroups - 1 time in 6 months (according to indications more often), persons from the III and IV groups - 1 time in 6 months.
2. Additional studies required during chemotherapy are defined in the relevant instruction (Appendix 8 to this order).
3. All patients with pyuria, hematuria and albuminuria produce three-time urine studies on MBT.
Anti-tuberculosis institutions
Zero Group - (0)
In the zero group, children and adolescents are observed to clarify the nature of positive sensitivity to tuberculin and / or for differential-diagnostic measures to confirm or eliminate tuberculosis of any localization.
First Group - (I)
In the first group, the patients with active forms of tuberculosis of any localization, highlighting 2 subgroups:
first-a (i - a) - patients with common and complicated tuberculosis;
first-b (i - b) - Patients with small and uncomplicated tuberculosis forms.
Second group - (II)
In the second group, observed patients with active forms of tuberculosis of any localization with the chronic course of the disease. Patients can be observed in this group in the continuation of treatment (including individual) and more than 24 months.
Third Group - (III)
In the third group, children and adolescents are taken into account with the risk of recurrence of tuberculosis of any localization . It includes 2 subgroups:
third-A (III-A) - first identified patients with residual posttuberculosis changes;
third-b (III-b) - Persons translated from I and II groups, as well as III-A subgroups.
Fourth Group - (IV)
In the fourth group, children and teenagers are in contact with sources of tuberculosis infection. It is divided into 2 subgroups:
fourth-A (IV-A) - individuals from family, related and apartment contacts with bacteriasels, as well as from contacts with bacteriasels in children's and adolescent institutions; Children and adolescents living in the territory of tuberculosis institutions;
fourth-b (IV-b) - Persons from contact with patients with active tuberculosis without bacteries; From family of livestock breeders working on dysfunctional on tuberculosis of farms, as well as from families having patients with tuberculosis of farm animals.
Fifth group - (V)
In the fifth group, children and adolescents are observed with complications after anti-tuberculosis vaccinations. Highlight 3 subgroups:
fifth - A (V-A) - patients with generalized and common defeats;
fifth-b (V-b) - patients with local and limited lesions;
fifth - in (V-B) - Persons with inactive local complications, both for the first time identified and translated from V-A and V-B groups.
Sixth Group - (VI)
In the sixth group, there are persons with elevated risk of local tuberculosis. It includes 3 subgroups:
sixth-A (VI-A) - children and adolescents in the early period of primary tuberculosis infection (turning tuberculin reactions);
sixth-b (VI-b) - previously infected children and adolescents with a hypeergic reaction to tuberculin;
sixth-in (VI-B) - Children and adolescents with amplifying tuberculin sensitivity.
The procedure for dispensary observation and accounting for children's and adolescent contingents of anti-tuberculosis institutions is presented in Table. 3.
Table 3.
The procedure for dispensary observation of contingents of children and adolescents, registered with the tuberculosis institutions of the Russian Federation
| Group / Subgroup accounting | Characteristics of contingents | The frequency of visits to a doctor with a patient or a patient by a doctor | Term of observation in the accounting group | Medical - diagnostic and preventive measures | Dispensary Observation Efficiency Criteria | |
| Zero group | ||||||
| Children and adolescents needing: - in clarifying the nature of tuberculin sensitivity; - in the diagnosis and clarification of the activity of tuberculosis. | Determined by the diagnostic technique. | Not more than 3 months. | A complex of diagnostic methods (in a hospital or dispensary). | Diagnosis of activity of tuberculosis changes in respiratory organs. Establishing the diagnosis or etiology of allergies to tuberculin. | ||
| First Group (Active Tuberculosis) | ||||||
| I-A. | Patients with common and complicated tuberculosis. | With outpatient treatment - at least 1 time in 10 days, after stationary or sanatorium treatment - at least 1 time per month. | Not more than 24 months from the date of registration. | Comprehensive main course of treatment; In the presence of testimony - surgical treatment, sanatorium treatment. Visiting a common school is permitted only after the end of the main course of treatment. | Translation into group II is no more than 10% of all patients with active tuberculosis. Translation into an III-B subgroup of persons with tuberculous intoxication, limited processes and small forms of tuberculosis in 95% of cases in terms of up to 9 months. No mortality from tuberculosis. | |
| I-B. | Patients with small and uncomplicated tuberculosis forms. | Not more than 9 months from the date of taking into account. | ||||
| Second group (active tuberculosis with chronic current) | ||||||
| II. | Patients with chronic flow tuberculosis in need of continuing treatment. | Determined by the condition of the patient and the treatment carried out. | Individualized complex chemotherapy, taking into account the medicinal sensitivity of the MBT, surgical and sanatorium treatment, additional wellness activities. Visiting a common school is not permitted. | Translation of 80% of patients in the III-B subgroup after 12 months. | ||
| Third Group (Risk of Tuberculosis Recurious) | ||||||
| III-A. | For the first time identified persons with residual posttuberculosis changes. | At least 1 time in 3 months; During the period of anticorcidal courses - depending on the methods of their conduct. | Not more than 12 months. | Integrated examination at least 1 time in 6 months. Conducting anti-infertion courses of chemotherapy - according to the testimony. Events on socio-labor rehabilitation. Visiting a common school is allowed. | Lack of tuberculosis reactivation. Translation under the supervision of the polyclinic of the general treatment network at the place of residence of 90% of the contingent III group after 24 months. | |
| III-B. | Persons translated from I, II, III-A groups. | No more than 24 months Persons with pronounced residual changes translated from I and II groups are observed before transferring to the dispensary department for adults. | ||||
| Fourth Group (Contacts) | ||||||
| IV-A. | - Children and adolescents of all ages, consisting in domestic (family, related, apartment) contact with patients with an active form of tuberculosis with bacteria, as well as with bacteria detectors identified in children's and adolescent institutions - children and adolescents living in the territory of tuberculous institutions. | No less often 1 time in 6 months. In the period of preventive treatment - depending on the methodology for its conduct. | The entire period of contact and at least 1 year from the time of the cessation of the activity of the tuberculosis process in the patient. For those in contact with the sick died of tuberculosis - 2 years. | Comprehensive examination 2 times a year. The mode and methods of chemotherapy are determined individually taking into account the risk factors. Structuring activities that contribute to improving immunity, incl. Sanatorium treatment. | Lack of tuberculosis in the process of observation and within 2 years after preventive measures. | |
| IV-B. | Children from contact with patients with active tuberculosis without bacteria. Children from livestock families working on dysfunction on tuberculosis of farms, as well as families having patients with tuberculosis of farm animals. | |||||
| Fifth group (complications after anti-tuberculosis vaccinations) | ||||||
| V-A. | Patients with persistent and disseminated BCG infection, including damage to the bone-screen system, purulent occasional lymphadenitis (with lesion 2 or more groups). | Determined by the condition of the patient and the treatment carried out, but at least 1 time in 10 days. | The duration of observation is not limited. | Comprehensive main course of treatment. In the presence of testimony - surgical treatment. Medical and social rehabilitation activities. A visit to common children's institutions is permitted. | Translation into V-to group 20% of all first identified patients. Achieving medical and social and labor rehabilitation. | |
| V-B. | Patients with limited and local lesions: purulent-occasional lymphadenitis of one group, lymphadenitis without fistula, cold abscess, ulcer, infiltration size more than 1cm, -rifying keloid scar. | Determined by the condition of the patient and the treatment carried out, but at least 1 time per month. | Not less than 12 months. | |||
| V-V- | Persons with inactive BCG infection: - for the first time identified lymphadenitis in the calcination phase, not a growing keloid scar; -Transmitted from V-A and V-B groups. | No less often 1 time in 6 months. In the period of preventive treatment, it is determined by the methodology for its implementation. | The duration of observation is not limited. | |||
| Sixth group (increased risk of tuberculosis) | ||||||
| VI-A. | Children and teenagers in the early period of primary tuberculosis infection (turning tuberculin reactions). | No less often 1 time in 6 months. During the treatment period, it is determined by the methodology for its conduct. | Not more than 1 year. In the presence of medical and social risk factors, as well as for persons in contact with the patients, died of tuberculosis - 2 years. | Comprehensive examination 2 times a year. The mode and methods of chemotherapy are determined individually taking into account the risk factors. | Lack of tuberculosis diseases. | |
| VI-B. | Children and adolescents previously infected with a hypergic reaction to tuberculin. Children and adolescents from social risk groups with severe reactions on Tuberculin. | |||||
| VI-B. | Children and teenagers with amplifying tuberculin sensitivity. | |||||
Notes.
1. When identifying active tuberculosis, turning tuberculin reactions and hyperergia in children and adolescents, it is necessary to examine all family members within 2 weeks.
2. The medical and social risk factors are: the absence of BCG vaccination at birth, concomitant chronic pathology, the presence of the source of sustainable strains of MBT, socio-deedapoted, large, low-income families, migrants and refugees.
3. Children and adolescents from I-A groups can be admitted to the teams in the presence of the following mandatory criteria: pronounced positive dynamics; The absence of mycobacterium tuberculosis with bacterioscopic studies and 3-multiple negative crops on mycobacteria tuberculosis; Closing disintegration cavities.
4. Persons who have revealed the increase in tuberculin sensitivity during the first 3 months. observed in a zero group. In the VI-in group of accounting, they are translated only with further increasing sensitivity or presence of medical and social risk factors.
5. Patients with active tuberculosis in the presence of anamnesis, clinical and radiological and other data indicating communication with anti-tuberculosis vaccination are observed in V-A and V-B metering groups. In the V-to group, they are translated after cure only while maintaining residual posttuberculous changes.
6. In I-A, the accounting group is isolated patients with a decay of lung tissue and bactering.
7. Residual posttuberculosis changes in respiratory bodies in children and adolescents are defined as:
-Theless: single calcinates in lymph nodes and lungs, fibrosis within one segment;
-Meriously pronounced: small calcinates in several groups of lymph nodes, a group of dense and calcined foci in the lungs, fibrosis within the share of or 1-2 segments in both lungs;
-pronounced: Massive calcination in several groups of intragenic lymph nodes, foci in the lungs, pneumosclerosis in 2-3 dollars or in 1 share with the presence of bronchiectasis.
Table 4.
Wednesday Thursday -
Friday -
Date of issuing notification _________________
Chairman of the CVKK (KEK) __________________________
Appendix No. 2.
to the organization's instructions
dispensary observation and accounting
contingents anti-tuberculosis
institutions
Notification number ______
on the removal from the accounting of the anti-tuberculosis institution
Dear (AA) __________________________________!
Central doctor
According to the materials of V.
What is tuberculosis?
This is a disease that is caused by bacteria called Mycobacterium tuberculosis. This bacterium is usually affecting the lungs, but sometimes it can also affect other organs: kidneys, spine, brain. In case of improper treatment, this disease can become deadly. At a certain period, tuberculosis was the leading cause of death in the United States.
Tuberculosis spreads from one person to another air-droplet. The bacteria get into the air when a person, a sick active form of tuberculosis of the lungs or throats cough, sneezes, says or sings. People who are near, can inhale these bacteria and thus become infected.
However, not everyone who is infected with bacteria tuberculosis is ill. People who are infected, but are not sick, have the so-called latent tuberculosis. Such people do not feel sick, do not have any symptoms and cannot infect someone else to the tuberculosis. However, some of them can develop with tuberculosis in time.
There are good news. People with the active form of tuberculosis can be cured if you have medical care in time. Moreover, most people with a latent form of tuberculosis should also take medical preparations to prevent the development of the active form of tuberculosis.
Why does the incidence of tuberculosis remain a problem in modern society?
At the beginning of the twentieth century, Tuberculosis killed every seventh resident of the United States and Europe. Only at the beginning of the 40s of the twentieth century was developed the first of the medicines that are used today in the treatment of tuberculosis. As a result, the incidence rate of tuberculosis began to gradually decrease. In the 70s and early 80s, a positive trend was prespicing the vigilance of specialists, and measures to combat tuberculosis were mitigated. This error led to a new surge in the incidence of tuberculosis in 1985-1992. Nevertheless, the increase in financing and increasing attention to the problem of tuberculosis made it possible to reduce the prevalence of this disease since 1993.
However, tuberculosis is still a problem. For example, the number of new cases of tuberculosis diagnostics continues to decline, but the speed of this decline has slowed down since 2003. Tuberculosis with multiple drug resistance (TB-MDU) is still concerned, and everything is more relevant to the problem of tuberculosis with broad drug resistance (Slo-TB).
We present answers to the most common questions about Tuberculosis. If you have any additional questions, you should consult a doctor.
How does tuberculosis spread?
Tuberculosis is transferred from man to man by air-droplet. Bacteria enters the air when the patient's active form of tuberculosis of the lungs or throat coughs, sneezes, says or sings. People who are near, can inhale these bacteria and thus become infected.
When a man inhales tuberculosis bacteria, they can settle in the lungs and begin to multiply. From here through blood they can get into the kidneys, spine, brain.
Tuberculosis of the lungs or throat can be infected, that is, can be transmitted to other people. Tuberculosis of other organs and parts of the body, such as kidneys or spine, is usually not infected.
People with the active form of tuberculosis are most likely to enter into those who are near them constantly: family members, friends, employees or classmates.
What is a latent form of tuberculosis?
Most people who inhale tuberculosis bacteria are infected in this way, the body is able to fight these bacteria and prevent their reproduction. Bacteria become inactive, but remain living in the body and over time they can become active again. This is called the latent form of tuberculosis.
Latent tuberculosis media:
- do not have symptoms
- do not feel painful
- can't infect others
- usually have a positive result of intradermal sample or blood test for tuberculosis,
- can acquire the active form of tuberculosis if it is not treated with its latent form.
Many people having a latent form of tuberculosis, the disease never develops in an active form. These people have bacteria remain inactive throughout life, without causing the development of the active form of the disease. Other people, especially those whose immune system weakened, bacteria are activated, multiplied and cause tuberculosis.
What is the active form of tuberculosis?
Bacteria tuberculosis become active if the body's immune system is not able to stop their growth. Active bacteria begin to multiply in the body and cause the active form of tuberculosis. Bacteria attack the body and destroy the tissues. If this happens in light, bacteria can even make a hole in it. In some people, the active form of tuberculosis develops shortly after the moment of infection (within a few weeks), before the immune system, the tuberculosis bacteria can be defeated. Other people may get sick years after infection, when their immune system will weaken for one or other reasons.
The decrease in immunity is characteristic of infants and small children, as well as for people infected, which causes AIDS, and other people with the following conditions:
- psychoactive abuse,
- head Cancer or Neck
- or Hodgkin's disease,
- some kidney diseases,
- low weight
- certain drug treatment (for example, therapy with corticosteroids or drugs that are used to prevent the rehabilitation of the transplanted organ after transplantation),
- specialized treatment of rheumatoid arthritis or crown disease.
Symptoms of tuberculosis depend on which part of the body bacteria multipliate. Tuberculosis in the lungs can cause the following symptoms:
- strong cough that does not stop for three weeks and longer,
- pain in the chest,
- or sputum.
- weakness and increased fatigue,
- weight loss without visible reasons
- lack of appetite,
- fever
- increased sweating at night.
The difference between the latent form of tuberculosis and the active form of tuberculosis
|
Man with a latent tuberculosis form |
Man with an active form of tuberculosis |
|
Does not feel ailment |
Usually feels ailment |
|
No symptoms |
It has symptoms that may include: Strong cough that does not stop for three weeks and longer, Pain in the chest, Cough with blood or sputum. Other symptoms of the active form tuberculosis include: Weakness and increased fatigue, Weight loss without visible reasons Lack of appetite, Fever Increased sweating at night. |
|
Not contagious for others |
Infectious for others |
|
Usually have a positive result of intradermal sample or blood test for tuberculosis |
|
|
X-ray does not identify pathology, tuberculosis sputum analysis |
Radiography can identify pathology, a sputum analysis or her sowing may be positive |
|
Tuberculosis latent infection should be treated to prevent the development of the active form of the disease. |
Need to treat the active form of the disease |
Vladislav
Tried breathing problems. I do not know how to describe this condition correctly, but if in your own words, then the feeling as if I can't breathe with a full breast (there is no feeling of saturation by air, as if I want to zajnut, but I can not).
Against this, I went to the fluorography. Fluorography conclusion:
"In the projection of C1-2 segments, a group of middle density centers is traced on the left. There is also moderate deformation of the vascular.
Otherwise, the pulmonary fields are transparent, the pulmonary pattern is not changed. The roots are structural, not expanded.
The median shadow of the usual configuration is not extended, not shifted.
The diaphragm is usually located with a clear level contour. Sinuses are free.
Recommended comparison with previous studies, consultation of the phthisiator, according to the testimony - Conducting the MSCT of the study. "
Immediately from fright made MSCT. Conclusion MSKT:
"In the series CT of the chest organs, the airiness of both lungs are saved. The trachea, the main, equity and segmental bronchi are passable, the lumen is not narrowed, the walls are not thickened. The pulmonary figure is somewhat strengthened, deformed in S1-2 to the left due to the fibrous change zone of peribroscial, sublocral location. , minimally advanced bronchops (by type of bronchiectasis), with single calcinates up to 3mm in diameter. In the apical departments of the lungs, moderatety spikes. Lymphatic mediastone nodes permissible sizes. Pleural sheets are not thickened, liquids in pleural cavities and pericardial cavities are not. Heart in the progress Sizes, main vessels are not changed.
CONCLUSION: Valid changes in S1-2 on the left more likely a specific nature. "
With this, everyone I went to the PDD at the place of residence. Where did the Diskintest, which turned out to be a positive, 20mm papule.
Against this background, I was prescribed test therapy for two months, eremfat + pyrazinamide + isoniazid. Followed by CT.
It also passed the sputum including Genexpert, but it had more saliva than sputum, because It does not stand out. All negatively.
There was still a general blood test, biochemistry, everything is normal in them, only small changes in Lake. formula. I also handed over PCR blood on tuberculosis, it is also negative.
Now, after a month of treatment, he began to swash periodically, the feeling as if a shiny in his throat and want to cough, from which we were prescribed to wash the nose, isofra and lizobact (for 3 days it didn't seem to be particularly helped). Every day, closer to the evening the temperature rises to 36.9 on average a little more. And there is a feeling of burning on the skin of the back, and in general, on all the body, strange tingling.
What is the probability that this is still tuberculosis? What does "post-inflammatory changes in S1-2 on the left more likely a specific nature"? Can tuberculosis against the background of treatment progress? When registering that CT was made in September, how much did his picture change until today?
Tuberculosis, MBT or TB (reduction from tuberculous bacillus), in the past wearing the name of the charity, a tuberculus, or pearl, is a widespread and in many cases a fatal infectious disease caused by various strains of mycobacteria, usually by mycobacterium tuberculosis. Usually tuberculosis attacks the lungs, but can also affect any organ. It spreads through the air when a person who is an active tuberculous bacillus cough, sneezes or otherwise transfers respiratory fluids by air. Most of the infections have no symptoms and is known as latent tuberculosis. Approximately one of the ten latent infections will ultimately progress into an active disease, which, if remains unbearable, kills more than 50% of infected. Classic symptoms of active tuberculosis infection include chronic cough with blood wets, heat, night sweating and weight loss (the latter gave the basis for a previously used name of the disease, "Chakhotka"). An infection of other organs causes a wide range of symptoms. The diagnosis of active tuberculosis is raised by means of radiology (usually radiograph of the chest), as well as microscopic research and microbiological sample of body fluids. The diagnosis of latent tuberculosis is carried out by means of tuberculin skin sample (TST) and / or blood tests. Treatment is complex and requires the reception of many antibiotics over a long period of time. Social contacts are also checked and, if necessary, are treated. Antibiotic resistance is a growing problem with multiple drug resistance tuberculosis infections (MDR-TB). Prevention is based on mass surveys and vaccination using calcimete-gerin bacillos. One third of the world's population, presumably infected by mycobacterium tuberculosis, while a new infection occurs about 1% of the population every year. In 2007, the estimated 13.7 million chronic cases around the world were active, while in 2013, according to settlements, there were 9 million new cases. In 2013, it was observed from 1.3 to 1.5 million death-related deaths, most of which arose in developing countries. The total number of cases of tuberculosis decreased since 2006, and the number of new cases decreased after 2002. The prevalence of tuberculosis in various regions varies around the world; About 80% of the population of many Asian and African countries have positive results of tuberculin samples, while a positive result has only 5-10% of the US population. More and more people in developing countries are infected with tuberculosis due to the weak immune system, which is mostly associated with the high prevalence of HIV infection and the corresponding development of AIDS.
Signs and symptoms
Tuberculosis can infect any part of the body, but most often occurs in the lungs (known as pulmonary tuberculosis). Empty tuberculosis occurs when tuberculosis develops outside the lungs, although equally can coexist with the tuberculosis of the lungs. The main features and symptoms include heat, chills, night sweats, loss of appetite, weight loss and fatigue. Also largely can be observed symptom of drum sticks.
Pulmonary
If the tuberculosis infection becomes active, it most often covers the lungs (about 90% of cases). Symptoms may include breast pain and prolonged cough with sputum production. Approximately 25% of people have no symptoms (that is, they remain "asymptomatic"). Rarely, people can pump off the blood in small quantities, and in very rare cases the infection can destroy the pulmonary artery or aneurysm of Rasmussen, which leads to massive bleeding. Tuberculosis can become a chronic disease and cause an extensive scarring in the upper pieces of the lungs. The upper lobes of the lungs are more often susceptible to tuberculosis than the bottom. The cause of these differences is not completely clear. This can be connected either with the best stream of air, or with low lymphaticine in the upper pieces of the lungs.
Extligacy
In 15-20% of the active cases, the infection extends beyond the lungs, causing other types of tuberculosis. They are jointly designated as "extrapulic tuberculosis." Empty tuberculosis most often occurs in people with low immunity and young children. In the suffering HIV, it arises in more than 50% of cases. In particular, the places of occurrence of an extravalic infection include the pleura (tuberculous pleurisy), the central nervous system (tuberculosis meningitis), the lymphatic system (neck croftolez), a urinary system (tuberculosis of the urogenital tract), as well as bones and joints (spine tuberculosis), among others. When it applies to the bone, it is also known as "bone tuberculosis", the form of osteomyelitis. In some cases, the tear of the tuberculosis abscess through the skin leads to tuberculosis ulcers. A ulcer, which originates from the located near the infected lymphatic node, is painless, slowly increases and has an outdoor view of "suede". Potentially more serious, widespread form of tuberculosis is called "disseminated" tuberculosis, also widely known as miliar tuberculosis. Miliary tuberculosis covers up to 10% of extralling cases.
The reasons
Mycobacteria
The main cause of tuberculosis is to mycobacterium tuberculosis, small, aerobic, fixed bacillos. The high content of lipids of this pathogen explains many of its unique clinical characteristics. It is divided every 16-20 hours, which is an extremely slow speed compared to other bacteria, which are usually divided for less than an hour. Mycobacterium has a lipid bilayer of the outer membrane. If the gram is performed by gram, the tuberculosis mycobacterium is either painted very weakly as "gram-positive" or does not delay the paint as the result of the high content of lipids and mycolic acid in the cell wall. Mycobacterium tuberculosis can withstand weak disinfectants and survive in drought conditions for weeks. In nature, it can grow only in the cell of the host organism, but is amenable to cultivation in the laboratory. Using histological dyes with respect to the clefe samples of mucus (also wears the name "sputum"), scientists can see mycobacterium tuberculosis under a microscope. Since the tuberculosis mycobacterose retains certain strains even after treating with acidic solution, it is classified as acid resistant bacterium (AFB). The most common acid-resistant staining techniques includes a cyane-nielsen color, which stains acid-resistant bacteria bright red color, released on a blue background, as well as auramino-rhodamine color with subsequent fluorescent microscopy. The Tuberculosis Mycobacterium Complex (MTBC) includes four other causing tuberculosis mycobacteria: M. Bovis, M. Africanum, M. Canetti and M. Microti. M. Africanum is rarely found, but is a significant cause of tuberculosis in some regions of Africa. M. Bovis was once a frequent cause of tuberculosis, but the introduction of pasteurized milk to a large extent eliminated it as a threat to public health in developed countries. M. Canetti is rare and limited to an African horn, although a small number of cases was observed in African emigrants. M. Microti is also rarely found and is mainly observed in people with immunodeficiency, although the prevalence of this pathogen may have been significantly understated. Other known pathogenic mycobacteria include M. Leprae, M. Avium and M. Kansasii. The last two species are classified as "netuberculosis mycobacteria" (NTM). Nonuberculosis mycobacteria do not cause tuberculosis nor leper, but are the cause of pulmonary diseases that are reminded of tuberculosis.
Risk factors
Several risk factors make people more predisposed to tuberculosis infection. The most important worldwide risk factor is presented with HIV; 13% of all people with tuberculosis are infected with the virus. In particular, it represents the problem in subsacharan Africa, where the prevalence of HIV is quite high. As for people without HIV infected with tuberculosis, approximately 5-10% develop an active disease during life; For comparison, 30% at the same time infected HIV develops an active disease. Tuberculosis is closely related to overpopulation and malfunction, which makes it one of the main diseases of poverty. Thus, a group of increased risk includes: people who use prohibited substances, locals and workers engaged in places where vulnerable people are collected (for example, prisons and shelters for homeless), devoid of rights and unsecured resources of society, ethnic High risk minorities, children who were in close contact with patients of increased risk groups, as well as health workers serving such patients. Chronic lung disease is another substantial risk factor. Silicosis increases the risk of approximately 30 times. Smoking cigarettes have a roughly greater risk of developing tuberculosis compared to non-smoking. Other painful states can also increase the risk of developing tuberculosis. They include alcoholism and diabetes mellitus (threefold increase). Certain drugs, such as corticosteroids and infliximab (anti-αfno monoclonal antibodies), become risk factors of increased importance, especially in developed countries. There is also a component of genetic predisposition, the overall significance of which remains uncertain.
Mechanism
Broadcast
When people with active tuberculosis cough, sneeze, speak, sing or spit, they distinguish infectious aerosol drops with a diameter of 0.5 to 5.0 μm. For one sneeze, it can free up to 40,000 drops. Each of these drops can transmit the disease, since the infectious dose of tuberculosis is sufficiently small (inhalation of less than 10 bacteria can cause infection). People with long, frequent or close contact with people suffering from tuberculosis are in the group of particularly increased risk of infection, while the estimated percentage of infection is 22%. A person with active, but non-treated tuberculosis can infect 10-15 (or more) people per year. The transfer arises only from people with active tuberculosis - people with latent infection, presumably not contagious. The probability of transmitting an infection from one person to another depends on several factors, including the number of infected droplets thrown by the carrier, ventilation efficiency, the duration of exposure, the virulence of the strain of mycobacterium tuberculosis, the level of immunity of an uninfected person and others. The distribution cascade A person man can be avoided due to the effective isolation of people with active ("open") tuberculosis and formulate them on the diagram of adoption of anti-tuberculosis drugs. After about two weeks of effective treatment, subjects with an unstable active infection, as a rule, become unsuccessful for others. If someone is infected, usually required from three to four weeks before the first infected person becomes contagious enough to transmit the disease to others.
Pathogenesis
More than 90% of infected with tuberculosis infected with tuberculosis, that is, they have a latent tuberculosis infection (sometimes called LTBI), while only 10% have a chance that latent infection is progressing to open, active tuberculosis during life. People with HIV have the risk of developing active tuberculosis rises to about 10% per year. If effective treatment is not undertaken, the mortality rate for the cases of active tuberculosis is up to 66%. Tuberculosis infection occurs when mycobacterium reaches the lungs alveoli, where it invades and multiplies in endosomes of alveolar macrophages. Macrophages identify the bacterium as a foreign body and are trying to eliminate it with phagocytosis. During this process, the bacterium is wrapped with macrophage and is temporarily stored in a membrane-bound bubble, which is called the name of the phaginoma. The phagosome is then combined with a lysosome for the formation of phaglicosome. In the phagelicosome cell, the cell is trying to use oxygen and acid jet forms to kill the bacterium. However, mycobacteria of tuberculosis has a thin, amyloid capsule of mischievous acid, which protects it from these toxic substances. The mycobacterium tuberculosis is able to multiply inside the macrophage and ultimately kills the immune cell. The original focus of infection is in the lungs and is known as the "Gon Center", as a rule, is located either at the top of the lower line, or at the bottom of the upper part. Light tuberculosis can also result from infection from blood flow. The focus is known as the Symmon Center and is usually located in the upper part of the lungs. This hematogenous transmission can also disseminate infection into more distant places, such as peripheral lymph nodes, kidneys, brain and bones. All parts of the body can be subject to the disease, although, for unknown reasons, it rarely affects the heart, skeletal muscles, pancreas or thyroid gland. Tuberculosis is classified as one of the granulomatous inflammatory diseases. Macrophages, T-lymphocytes, B-lymphocytes and fibroblasts are connected, forming granulomas, with lymphocytes surrounding infected macrophages. When other macrophages attack infected macrophages, they are connected together, forming a giant multi-core cell in an alveolar cavity. Granuloma may prevent the spread of mycobacteria and provide a local medium for the interaction of the cells of the immune system. Nevertheless, more recent facts indicate that bacteria use a granule to avoid the destruction of the immune system of the host. Macrophages and dendritic cells in granulomas are not capable of presenting antigen to lymphocytes; Thus, the immune response is suppressed. Bacteria inside the granuloma can become inactive, causing a latent infection. Another property of granuloma lies in the development of pathological cell death (necrosis) in the center of tubercul. If you look with the naked eye, it has a soft, white cheese structure and is defined as curly necrosis. If tuberculosis bacteria fall into blood flow from damaged tissue, they can spread throughout the body and cause many foci of infection, all of which look like small, white tubercles in the tissues. This is a heavy shape of tuberculosis that is most common in small children and people with HIV, which is called miliar tuberculosis. People with such common tuberculosis have a high share of mortality even with treatment (about 30%). Many people have an infection overcoming and declining. The destruction of the fabric and necrosis is often leveled by healing and fibrosis. The touched fabric is replaced by scars and cavities filled with caseous curly material. During an active illness, some of these cavities join the respiratory tract of the bronchi and this material can be extended. It contains live bacteria, thus, can distribute infection. Treatment with appropriate antibiotics kills bacteria and allows healing. As a result of treatment, the affected areas are ultimately replaced by a scar cloth.
Diagnostics
Active tuberculosis
The diagnosis of active tuberculosis, based only on signs and symptoms, is difficult, since it is a diagnosis of the disease in those whose immunity is suppressed. The diagnosis of tuberculosis, however, should be taken into account among those whose symptoms of the disease of the lungs or systemic symptoms last two weeks. Radiograph of the chest and multiple sputum crops against acid-resistant bacilli are a typical part of the primary survey. Interferon-γ secretion tests and tuberculin skin tests have a slight application in developing countries. Interferon-Gamma release analyzes have similar restrictions on people with HIV. The final diagnosis of tuberculosis is raised as a result of the identification of mycobacterium tuberculosis in a clinical sample (for example, sputum, rowful or tissue biopsy). However, the impected cultivation process for this slow-growing organism can take from two to six weeks for sowing blood and sputum. Thus, treatment often begins before the presence of cultures in samples is confirmed. Tests based on the amplification of nucleic acids and adenosine administration testing can enable rapid diagnosis of tuberculosis. These tests are nevertheless not recommended in a planned manner, since they rarely affect human treatment. Blood tests for detecting antibodies do not have specificity or sensitivity, therefore, not recommended.
Latent tuberculosis
Manta Tuberculin Skin Sample is often used to check people in a group of high risk of development of tuberculosis. Those who have previously immunized can give a false positive result. The test result can be false negative in people with sarcoidosis, Hodgkin lymphoma, low failure, or, especially important, those who had true active tuberculosis. Interferon-Gamma secretion analyzes (IGRA) using blood samples are recommended for those who have a positive result of the Mantu sample. They did not undergo immunization or exposure to a large number of exogenous mycobacteria, thus give a smaller number of false positive results. However, they are exposed to M. szulgai, M. Marinum and M. Kansasii. The sensitivity of interferon-gamma secretion analyzes increases when used in addition to the skin sample, but they may be less sensitive than skin sample when used separately.
Prevention
Prevention of tuberculosis and management measures are mainly based on vaccination of newborns, as well as discovery and relevant treatment of active cases. The World Health Organization has achieved some success due to improved treatment schemes, as well as a minor reduction in the number of cases.
Vaccines
The only available vaccine according to 2011 is represented by Calmette Gena Bacillus (BCG). In children, it reduces the risk of infection with an increase of 20% and the risk of transition of infection into an active disease is about 60%. It is the most widely used vaccine on a global scale, while approximately 90% of all children are vaccinated. The immunity caused to it decreases after approximately ten years. Since tuberculosis is rarely found in most of Canada, Great Britain and the United States, BCG applies only to people in a group of increased risk. In part, the arguments against the use of the vaccine are that it makes a tuberculin skin sample of false positive, while not used when checking. To date, there are several new vaccines in the development.
Public Health
The World Health Organization declared tuberculosis "Threat to World Health" in 1993, and in 2006, in 2006, the Partnership for Combating Tuberculosis developed a global plan to combat tuberculosis, which aims to preserve 14 million lives from the period of its launch and until 2015 several The goals that he set before him are unlikely to be achieved until 2015, mainly due to the increase in the number of cases of HIV-conditioned tuberculosis and cases of multiple drug resistance tuberculosis. The system of classification of tuberculosis, developed by American thoracic society, is mainly used in public health programs.
Control
Antibiotics are used in the treatment of tuberculosis to destroy bacteria. Effective treatment of tuberculosis is difficult due to the unusual structure and chemical composition of the cell wall of mycobacteria, which prevents the penetration of drugs and makes many antibiotics ineffective. The two most widely used antibiotics are isoniazide and rifampicin, while treatment may be long and take several months. In the treatment of latent tuberculosis, one antibiotic is commonly used, while active tuberculosis is better to treat a combination of several antibiotics in order to reduce the risk that the antibiotic resistance will be reduced by bacteria. People with latent infections are also treated in order to prevent progression into active tuberculosis later. Treatment under direct supervision, for example, a medical worker who observing the reception of the patient of drugs is recommended to be WHO as a measure to reduce the number of people who do not take antibiotics properly. Evidence in support of this practice compared to people, independently receiving drugs, insufficient. Methods of reminders of people about the importance of treatment, however, it seems effective.
New episode
The recommended treatment for the first time detected pulmonary tuberculosis, according to 2010, is represented by the admission of combining antibiotics, including rifampicin, isoniazide, pyrazinamide and etcutol during the first two months, and receiving only rifampicin and isoniazid over the past four months. When the resistance to isoniazid is high, as an alternative to the last four months, etcutol can be added.
Recurd
When recurring tuberculosis before determining the treatment, testing is played for what antibiotic is sensitive. If multiple drug-resistant tuberculosis is revealed, treatment is recommended at least four effective antibiotics over 18 to 24 months.
Drug resistance
Primary stability occurs when a person is infected with a steady strain of mycobacterium tuberculosis. A person with a fully sensitive tuberculosis can develop secondary (purchased) stability during therapy due to inadequate treatment, improper compliance with the prescribed treatment regimen (non-compliance with the patient's instructions) or the use of low-quality drugs. Drug-resistant tuberculosis is a serious public health problem in many developing countries, since its treatment is long and requires more expensive drugs. Tuberculosis with multiple drug resistance is defined as resistant to the two most effective anti-tuberculosis preparations of the first line: rifampicin and isoniazid. Tuberculosis with extended drug resistance is also resistant to three and more of six classes of antibiotics of the second line. Tuberculosis with full drug sustainability is resistant to all the drugs to date. It was first revealed in 2003 in Italy, but it was often not reported until 2012, was also observed in Iran and India. Badquilin is experimentally used in the treatment of tuberculosis with multiple drug resistance. XDR-TB is a concept, in some cases used to determine tuberculosis with extended stability, while it constitutes one of ten cases of tuberculosis with multiple drug resistance. Cases of tuberculosis with extended drug resistance were detected in more than 90% of countries.
Forecast
The risk of renewal increases when the immunity is suppressed, such as caused by HIV infection. In people simultaneously infected with mycobacterium tuberculosis and HIV, the risk of renewal increases to 10% per year. Studies used by DNA genotiposcopy of strains of mycobacterium tuberculosis have shown that re-infection is more facilitated by the recurrence of tuberculosis than previously expected, according to calculations, this may cover more than 50% of the resumption cases in the regions where tuberculosis is widespread. The chance of death from tuberculosis is approximately 4% as of 2008, decreasing from 8% in 1995
Epidemiology
Approximately one third of the world's population is infected with mycobacterium tuberculosis, while a new infection occurs approximately 1% of the population every year. Nevertheless, most of the infections of the mycobacterium tuberculosis does not cause tuberculosis, while 90-95% of infections remain asymptomatic. In 2012, the estimated 8.6 million chronic cases were active. In 2010, 8.8 million new cases of tuberculosis were diagnosed, while 1.20-1.45 million deaths were observed, most of which arose in developing countries. Of these 1.45 million deaths about 0.35 million are infected with HIV. Tuberculosis is the second most common cause of death against infectious diseases (after associated with HIV / AIDS). Since 2005, the total number of tuberculosis has decreased since 2005, while the number of new cases decreased since 2002. China, in particular, has achieved significant progress in the form of approximately 80% of the decline in mortality share from 1990 to 2010. The number of new cases has decreased by 17 % in the period 2004-2014 Tuberculosis is more common in developing countries; Approximately 80% of the population in many Asian and African countries have positive results of tuberculin samples, while only 5-10% of the US population have positive results. Hopes for complete control of the disease were sharply destroyed due to several factors, including the difficulty of developing an effective vaccine, expensive and requiring time the diagnostic process, the need for a multi-month treatment, an increase in the number of cases of HIV-conditioned tuberculosis, as well as the emergence of drug-sustainable cases in the 1980s. In 2007, Swaziland was the country with the highest settlement occurrence of tuberculosis with a value of 1200 cases per 100,000 people. India has the greatest overall occurrence with the estimated value of 2.0 million new cases. In developed countries, tuberculosis is less common and found mainly in urban areas. Values \u200b\u200bper 100,000 people in different regions of the world were: on global scale 178, Africa 332, America 36, \u200b\u200bEast Mediterranean 173, Europe 63, Southeast Asia 278 and Western Pacific 139 according to 2010 in Canada and Australia Tuberculosis Long The time was distributed to the indigenous people, especially in remote areas. In the USA among the indigenous Americans, a large mortality from tuberculosis was observed in five, and racial and ethnic minorities cover 84% of all reported cases of tuberculosis. The prevalence of tuberculosis changes with age. In Africa, Tuberculosis is primarily susceptible to teenagers and young people. However, in countries where the occurrence was sharply reduced (such as the USA), tuberculosis mainly represents the disease of the elderly and people with weakened immunity (risk factors are listed above). On a global scale, 22 "especially painful" states or countries encompass 80% of cases, as well as 83% of deadly outcomes.
History
Tuberculosis was found in people from the time of antiquity. The earliest accurate detection of mycobacterium tuberculosis is evidence of the presence of a disease in the remains of the Bizon in Wyoming, which are dating about 17,000 years ago. Nevertheless, whether tuberculosis occurs from ruminant animals, passed by a person, or he went away from the general predecessor, today it is not clear. Comparison of Tuberculosis mycobacteria complexes (MTBC) in people with MTBC in animals indicates that people did not receive MTBC from animals in the process of domestication, as stated earlier. Both strains of tuberculosis bacteria have a common predecessor who infected a person already during the Neolithic Revolution. Skeletal remains showed that prehistoric people (4000 years BC) had tuberculosis, and the researchers discovered tuberculous decomposition in the spines of Egyptian mummies dating from 3000-2400. BC. Genetic studies show that tuberculosis existed in America from about 100 AD. Tuberculosis is a Greek word for the designation of consumers, an old concept for describing the lung tuberculosis; About 460 BC. Hippocrates recognized tuberculosis as the most common disease of all time. As mentioned, he manifested itself like a heat and expectoration of blood and was almost always fatane. The folklore has often connected tuberculosis with vampires to the industrial revolution. When one family member died from tuberculosis, other infected family members slowly lost their health. People believed that this was caused by the fact that the first died of tuberculosis sucking life from other family members. Although the pulmonary form associated with tubercles was determined as a pathology Dr. Richard Morton in 1689, due to a multitude of symptoms, tuberculosis was not recognized as a separate disease until the 1820s. He did not wear Tuberculosis titles until 1839, until he was named as J. L. Shenglein. In the period from 1838 P1845, Dr. John Krogan, the owner of the mammoth cave, led several people with tuberculosis in the cave in the hope of cure the disease due to a constant temperature and pure cave air; They died throughout the year. Herman Bremer opened the first tuberculous sanatorium in 1859 in Herbersdorf (in our days Sokolovo), Silesia. Bacillus, causing tuberculosis, Tuberculosis mycobacterium, was discovered and described on March 24, 1882 by Robert Koh. For his opening, he received the Nobel Prize in Physiology and Medicine in 1905 Koh did not believe that tuberculosis of cattle and human was the same, which prevented the determination of infected milk as a source of infection. Later, the risk of transmission from this source was dramatically reduced due to the invention of the process of pasteurization. Koh declared the glycerin extract of tuberculosis bacillos as a "medicine" from tuberculosis in 1890, giving him the name "Tuberculin". While it was not effective, later it was successfully adapted as a check test for preimmptomatic tuberculosis. Albert Calmette and Camille Herern reached the first real success in immunization against tuberculosis in 1906, using weak strains of cattle tuberculosis. The vaccine was named Bacillus Calmette-Geren (BCG). The vaccine was first used in respect of a person in 1921 in France, but was widely appreciated in the United States, Great Britain and Germany only after World War II. Tuberculosis caused the strongest public concern in the XIX and early XX centuries as an endemic disease of the city poverty. In 1815, one of the four deaths in England was associated with "Cachotka". Until 1918, one of the six deaths in France was also caused by tuberculosis. After it was revealed that tuberculosis is infliced, in the 1980s, it was introduced to the list of diseases subject to mandatory registration in the UK; Campaigns were launched in order to prevent sneezing in public places, and infected poor people "strongly recommended" the admission to the sanatoriums, who reminded prisons (sanatoriums for secondary and higher classes offered excellent medical care and continuous monitoring of medical personnel). Despite (presumatively) the benefit of "fresh air" and sanatorium workers, even in the best conditions, 50% of the sanatorium arrived in the sanatorium for five years (about 1916). In Europe, the prevalence of tuberculosis began to grow at the beginning of the 1600s and reached a peak level in the 1800s, when tuberculosis caused about 25% of all deaths. Until the 1950s, mortality was reduced by about 90%. Improvements in the field of public health began significantly reduced the prevalence of tuberculosis even before the appearance of streptomycin and other antibiotics, although the disease remained a significant threat to public health to such an extent that when the Great Britain was formed by the Medicine Research Council in 1913, his attention was aimed. First of all, on the study of tuberculosis. In 1946, the development of an antibiotic streptomycin made effective treatment and healing from tuberculosis with reality. Prior to the introduction of this drug, the sole treatment (with the exception of sanatoriums) was a surgical operation, including the "pneumothorax procedure", which includes the compression of the infected lung to the state of "rest", which gave the opportunity to heal a tuberculous damage. Due to the urgent nature of multiple drug resistance tuberculosis, surgical intervention was re-introduced as an additional method of treatment within the framework of the generally accepted standard in the treatment of tuberculosis infections. Today, surgical operations include the removal of pathological infants ("Bull") in the lungs in order to reduce the amount of bacteria and the effects of the remaining bacteria on drugs in the bloodstream, thus, at the same time, reducing the overall bacterial load and increasing the efficiency of systemic therapy with antibiotics. Hopes for the complete elimination of tuberculosis (CP. OPE) among the population were destroyed after the growth of the number of drug-resistant strains in the 1980s. The subsequent revival of tuberculosis led to the emergence of a declaration about the threat of global health protection from the World Health Organization in 1993
Society and culture
Public health measures
World Health Organization, Bill and Melinda Gates Foundation, as well as the US government allocated subsidies for high-speed diagnostic tests for tuberculosis for use in low- and middle-income countries. In addition to rapid action, the test could determine whether there is a resistance to antibiotic rifampicin, which helped recognize tuberculosis with multiple-resistant drugs, and also gave accurate results for those who were simultaneously infected with HIV. Many people unsecured by the resources according to 2011 had access only to sputum microscopy. India had the maximum number of cases of tuberculosis on a global scale in 2010, in particular, due to poor control of the disease within the framework of personal and public health. Programs, such as the revised National Tuberculosis Anti-Tuberculosis Program, operate in order to reduce the incidence of incidence among people contacting the public health system. The report on the health care of the company "Economist Intellesen Unit" discussed indifference and appealed to an increase in financing. The report brought among the other words to the human trays "[tuberculosis] is similar to the orphan. It is deprived of attention even in countries with a high level of prevalence of the disease and is often neglected by donors and investors in the field of health. " Slow progress led to disappointment, expressed by the Executive Director of the Global Fund to Combat AIDS, Tuberculosis and Malaria - Mark Dibul: "We have the means to put an end to tuberculosis as a pandemic threat and a threat to public health on the planet, but do not do it." Several international organizations achieved greater transparency in treatment, and more and more countries gave mandatory to execute the government, although their observance is often superficial. Commercial treatment suppliers can often be overloaded with the preparations of the second line, as well as additional treatments, contributing to demand for further regulation. The Brazilian government provided universal medical care for tuberculosis, which facilitated this problem. On the contrary, the fall in the prevalence of tuberculosis infection may not be associated with the number of programs aimed at reducing the degree of prevalence of infection, but can be attributed to an increased level of education, income and public health. The cost of the disease, as was calculated by the World Bank in 2009 may exceed 150 billion USD per year in the countries "with a high prevalence of the disease." The lack of progress in the eradication of the disease can also be associated with a lack of observation of patients - both among 250 thousand rural migrants in China.
Social rejection
Research
Bacillus Calmette-Geren has limitations, while studying is constantly underway to develop a new vaccine against tuberculosis. Several potential candidates are currently in phase I and II clinical studies. In an attempt to improve the efficiency of available vaccines, two approaches are applied. The first approach includes the addition to the Calmette-Herin Bacillus of the subunit vaccine, while another strategy is an attempt to create new and best living vaccines. MVA85A, an example of a subunit vaccine, is currently exposed to research in South Africa and is based on a genetically modified ospovaccine virus. There is hope that vaccines play a significant role in treating both latent and active disease. Encouraging further discoveries, researchers and political persons contribute to the introduction of new economic models of vaccine development, including premiums, tax breaks and preliminary obligations for future procurement. Several groups, including a tuberculosis partnership, South African initiative for the development of tuberculosis vaccine and the Global Foundation for the Aeros Anti-Tuberculous Vaccine, are involved in research. Among them, the Global Foundation for the Aerras Anti-Tuberculosis Vaccine received as a gift more than 280 million USD from the Bill and Melinda Gates Foundation for the development and licensing of an improved tuberculosis vaccine for use in countries with increased prevalence of the disease. Several drugs were investigated against tuberculosis, sustainable to many drugs, including Bedasquilin and Delamanid. Bedasquiline was approved by the Office for Food Control and Medicinal Products (FDA) At the end of 2012, the safety and efficiency of these agents is still not clear, since it is based on relatively small studies. However, the available data suggests that patients who took Bedasquilin in addition to standard therapy against tuberculosis, die five times more often than those that do not take a new drug, which led to the emergence of articles in medical journals raising health policy issues regarding What reason the FDA approved the drug and whether financial connections with the company producing Bedacavilin, which influenced the support of the doctors of this drug.
 What is a hot water supply of an apartment building
What is a hot water supply of an apartment building Water supply of an apartment building
Water supply of an apartment building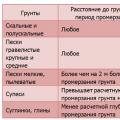 Calculation of the Load for the foundation Installed Electrical Instruments
Calculation of the Load for the foundation Installed Electrical Instruments