Abacavir lamivudine instructions for use. Medicinal reference book geotar. Release form and packaging
Russian name
Abacavir + LamivudineLatin name of substances Abacavir + Lamivudine
Abacavirum + Lamivudinum ( genus. Abacaviri + Lamivudini)Pharmacological group of substances Abacavir + Lamivudine
Use during pregnancy and lactation
Model clinical and pharmacological article 1
Pharma action. Combined antiviral (HIV) agent, nucleoside reverse transcriptase inhibitor, potent selective inhibitor of HIV-1 and HIV-2. Abacavir and lamivudine are metabolized by intracellular kinases to the corresponding triphosphates, which act as active metabolites. Lamivudine triphosphate and carbovir triphosphate (the active triphosphate of abacavir) are competitive inhibitors of HIV reverse transcriptase. However, the main antiviral effect is due to the incorporation of monophosphate into the DNA chain, which breaks as a result. Triphosphates of abacavir and lamivudine have a significantly lower affinity for host cell DNA polymerases.
Pharmacokinetics. With mild liver failure (5-6 on the Child-Puge scale), AUC of abacavir increases by 1.89 times, T 1/2 - by 1.58 times. The AUC of individual metabolites does not change, but the rate of their formation and excretion decreases. In renal insufficiency, the AUC of lamivudine increases due to a decrease in clearance.
Indications. HIV (as part of combination therapy with other antiretroviral drugs).
Contraindications. Hypersensitivity, liver failure, chronic renal failure (CC less than 50 ml / min), simultaneous administration with zalcitabine, body weight less than 40 kg, children's age (up to 12 years), lactation.
Carefully. Age over 65 years, pregnancy (taking into account the expected benefit to the mother and the possible risk to the fetus).
Dosing. Inside, regardless of food intake, 600 mg of abacavir + 300 mg of lamivudine 1 time per day.
Side effect. In 5% of patients taking abacavir, a hypersensitivity reaction (including fatal) may develop, which often develops in the first 6 weeks from the start of the drug (after an average of 11 days) in the form of symptoms of multiple organ damage.
Almost all patients (with the exception of individual cases) showed an increase in body temperature and / or the appearance of a maculopapular rash or urticaria.
On the part of the skin: 10% or more - maculopapular rash or urticaria.
From the digestive system: 10% or more - nausea, vomiting, diarrhea, pain in the abdominal cavity, increased activity of "liver" enzymes; liver failure, ulceration of the oral mucosa.
From the respiratory system: 10% or more - shortness of breath, cough; sore throat, respiratory distress syndrome, respiratory failure.
From the nervous system: 10% or more - headache; paresthesia.
On the part of the hematopoietic organs: lymphopenia.
From the musculoskeletal system: 10% or more - myalgia; rarely myolysis, arthralgia, increased CPK.
From the urinary system: hypercreatinemia, renal failure.
Others: 10% or more - fever, feeling tired, malaise; edema, lymphadenopathy, decreased blood pressure, conjunctivitis, anaphylaxis.
Side effects of abacavir or lamivudine are grouped by frequency: very often (more than 1/10), often (more than 1/100 less than 1/10), less often (more than 1/1000 and less than 1/100), rarely (more than 1/10000 and less than 1/1000) and very rarely (less than 1/10000).
According to clinical studies.
Abacavir.
From the digestive system: often - nausea, vomiting, diarrhea.
From the side of metabolism: often - anorexia.
Other: often hypersensitivity, fever, apathy, fatigue.
Lamivudine.
From the nervous system: often - headache.
On the part of the hematopoietic organs: less often - neutropenia, anemia, thrombocytopenia.
From the digestive system: often - nausea, vomiting, pain in the upper abdominal cavity, diarrhea; less often - a temporary increase in the activity of ALT, AST.
On the part of the skin: often - a rash.
Other: often - a feeling of fatigue, malaise, fever.
post-registration data.
Abacavir.
From the digestive system: rarely - pancreatitis (a causal relationship with the drug has not been established).
On the part of the skin: often - a rash (without systemic symptoms); very rarely - exudative erythema multiforme (including Stevens-Johnson syndrome), toxic epidermal necrolysis.
Lamivudine.
From the nervous system: very rarely - paresthesia, peripheral neuropathy (causal relationship has not been established).
From the digestive system: rarely - increased activity of serum amylase, pancreatitis (causal relationship has not been established).
On the part of the hematopoietic organs: very rarely - true erythrocyte aplasia.
From the musculoskeletal system: often - arthralgia, muscle damage; rarely - rhabdomyolysis.
On the part of the skin: often - alopecia.
From the side of metabolism: often - hyperlactatemia, rarely - lactic acidosis.
With combined antiretroviral therapy, there is a redistribution / accumulation of body fat, the frequency of which depends on many factors (including the combination of antiretroviral drugs) and lactic acidosis.
Overdose. Symptoms: increased side effects.
Treatment: symptomatic, hemodialysis (to remove lamivudine).
Interaction. Abacavir and lamivudine are slightly metabolized by enzymes of the cytochrome P450 system (CYP3A4, CYP2C9, CYP2D6) and do not have an inhibitory or inducing effect on them, so the likelihood of interaction with antiretroviral non-nucleoside protease inhibitors and other drugs, the metabolism of which occurs with the participation of enzymes of the cytochrome P450 system, is low.
When taken simultaneously with ethanol, the AUC of abacavir increases by 41%.
When taking abacavir (600 mg 2 times a day) with methadone, C max of abacavir decreases by 35%, TC max increases by 1 hour, AUC does not change; methadone clearance is increased by 22%.
Administration of trimethoprim/sulfamethaxosole 160 mg/800 mg resulted in a 40% increase in lamivudine AUC.
Lamivudine inhibits intracellular phosphorylation of zalcitabine when they are taken simultaneously, significantly enhances the effect of zidovudine.
Abacavir enhances the effect of amprenavir, nevirapine and zidovudine. The effect of the drug is enhanced in combination with didanosine, zalcitabine, stavudine and lamivudine.
Special instructions. Treatment should be carried out by a physician experienced in the use of the drug.
The drug should not be used in cases where dose adjustment is necessary (CC less than 50 ml / min, liver failure) due to the presence of fixed doses of individual components in one tablet. In such cases, monotherapy with abacavir or lamivudine is carried out.
In 5% of patients taking abacavir, a hypersensitivity reaction is noted (more often in the first 6 weeks), which in rare cases is fatal. If symptoms of multiple organ involvement (fever and/or rash, weakness, malaise, nausea, vomiting, diarrhoea, abdominal pain, shortness of breath, sore throat, cough, chest x-ray evidence of lesions (infiltrates)) occur, stop and never resume taking the drug, as well as other drugs containing abacavir. The recurrence of the hypersensitivity reaction is more severe (compared to the first reaction) in nature and may be accompanied by a decrease in blood pressure (up to death).
The risk of developing a hypersensitivity reaction to abacavir is determined by a genetic factor (the presence of the HLA-B5701 allele), which is present in 50% of Caucasian patients, in 8% of Black patients and in 22% of patients of Hispanic ethnicity. However, the basis of diagnosis is the presence of clinical symptoms of a hypersensitivity reaction, regardless of whether the HLA-B5701 allele is present or not.
When taking the drug, it is possible to develop lactic acidosis, severe hepatomegaly with steatosis, incl. with a lethal outcome. The drug should be stopped even in the absence of a significant increase in transaminase activity.
In some patients, there is a redistribution of fat in the body: an increase in the back of the neck and back (“buffalo hump”), an increase in the mammary glands, a decrease in fat in the periphery and in the face. Perhaps the development of lipodystrophy, hyperglycemia and hyperlipidemia.
When prescribing the drug in patients with concomitant viral hepatitis B, liver function tests and markers of viral hepatitis B replication should be monitored.
When taking the drug, opportunistic infections and other complications of HIV may develop.
Patients resistant to abacavir have reduced sensitivity to lamivudine, zalcitabine, tenofovir, emtricitabine and/or didanosine, but remain sensitive to zidovudine and stavudine.
Development of cross-resistance between abacavir, lamivudine and antiretroviral drugs
Clinico-pharmacological group:Included in medications
Included in the list (Decree of the Government of the Russian Federation No. 2782-r dated December 30, 2014):VED
ATH:J.05.A.R.02 Abacavir + Lamivudine
Pharmacodynamics:Combined antiviral (HIV) agent, nucleoside reverse transcriptase inhibitor, potent selective inhibitor of HIV-1 and HIV-2. and are metabolized by intracellular kinases to the corresponding triphosphates, which act as active metabolites. However, the main antiviral effect is due to the incorporation of monophosphate into the DNA chain, which breaks as a result. Triphosphates of abacavir and lamivudine have a significantly lower affinity for host cell cDNA polymerases.
Pharmacokinetics:Screening for carriage of the HLA-B*5701 allele is recommended prior to re-administration of an abacavir-containing drug in patients with unknown HLA-B*5701 status who previously tolerated abacavir-containing drug therapy well.
The use of abacavir preparations is not recommended in such patients and should only be considered in exceptional cases under close medical supervision, when the potential benefit outweighs the risk of using the drug.
The clinical diagnosis of a suspected hypersensitivity reaction should remain the basis for the decision to use preparations containing , in all patients. Even in the absence of the HLA-B * 5701 allele, it should be discontinued and not resumed in all cases where a hypersensitivity reaction cannot be excluded based on clinical data, due to the potential risk of serious adverse effects or even death.
Clinical picture
The hypersensitivity reaction is characterized by the appearance of symptoms of multiple organ damage. Most patients present with fever and/or rash.
Other possible symptoms of hypersensitivity include: weakness, malaise, gastrointestinal symptoms (such as nausea, vomiting, diarrhea, abdominal pain), respiratory symptoms (such as shortness of breath, sore throat, cough), and x-ray signs lesions of the chest organs (mainly limited infiltrates). Symptoms of a hypersensitivity reaction during treatment with abacavir can occur at any time, however, as a rule, appear within the first six weeks of taking the drug. With continued treatment, the severity of symptoms increases, and they can become life-threatening. In most cases, these symptoms disappear when you stop taking abacavir.
Some patients with hypersensitivity initially thought they were suffering from respiratory (pneumonia, bronchitis, pharyngitis) or influenza-like illnesses, gastroenteritis, or reactions to other drugs. In this regard, the hypersensitivity reaction was not immediately diagnosed, and patients continued (or resumed) taking the drug. This entailed the development of a more severe hypersensitivity reaction (up to death). Taking this into account, it is necessary to take into account the possibility of developing such a reaction and exclude it in patients with symptoms of these diseases. If it is impossible to exclude the presence of a hypersensitivity reaction, you should not resume taking the drug or any other drug containing.
Hypersensitivity symptoms worsened with continued treatment and usually resolved after discontinuation of abacavir.
Restarting abacavir after a hypersensitivity reaction within a few hours results in a rapid return of symptoms. A relapse of a hypersensitivity reaction may be more severe than the first reaction and be accompanied by a life-threatening decrease in blood pressure (up to death). Patients who experience such a hypersensitivity reaction should stop and never resume taking the drug, as well as any other medicinal products containing.
There are isolated reports of the development of a hypersensitivity reaction after the resumption of abacavir, discontinued at the appearance of certain key symptoms of hypersensitivity (rash, fever, weakness / malaise, gastrointestinal disorders or respiratory symptoms). In very rare cases, the development of a hypersensitivity reaction has been reported after the resumption of the drug in patients who previously had no symptoms of hypersensitivity.
Treatment
Patients, regardless of HLA-B*5701 status, who develop signs and symptoms of hypersensitivity MUST contact their healthcare provider immediately for advice. If a diagnosis of hypersensitivity is made, the drug SHOULD be discontinued immediately. NEVER restart treatment with the drug and other medicinal products containing (such as Ziagen, Trizivir) after a hypersensitivity reaction has occurred. This is due to the risk of severe symptoms (including life-threatening hypotension) that can lead to death within a few hours after the resumption of the drug.
To prevent delayed detection and reduce the risk of life-threatening hypersensitivity, the drug should be completely discontinued if hypersensitivity cannot be ruled out, even with the potential presence of other diseases (respiratory diseases, influenza-like illness, gastroenteritis, reactions to other drugs). It is not necessary to resume treatment with the drug and other medicinal products containing (such as Ziagen, Trizivir), even if symptoms of hypersensitivity appear when other drugs are taken repeatedly.
Special instructions for treatment after a break in drug therapy
In case of discontinuation of treatment with the drug, regardless of the carriage of the HLA-B * 5701 allele, before resuming the drug, you should carefully study the reason for refusing to use the drug and make sure that the patient does not have symptoms of a hypersensitivity reaction. You should not resume taking the drug and other drugs containing, if it is impossible to exclude a hypersensitivity reaction.
A few cases of hypersensitivity reactions have been described when abacavir treatment is restarted after its withdrawal due to the appearance of any one of the typical symptoms of hypersensitivity (rash, fever, malaise, fatigue, gastrointestinal disturbances and respiratory system disorders). Since in all such cases a hypersensitivity reaction cannot be ruled out and, taking into account the data on its more severe course with repeated use of abacavir, the resumption of therapy with the drug or another containing drug in these patients is not recommended.
A hypersensitivity reaction has been observed, although extremely rare, even when treatment with this drug is resumed in patients who have not previously experienced symptoms of this reaction, and the interruption in taking the containing drug was associated with other reasons. In this case, the resumption of the drug is possible, but requires that the patient or people around him have quick access to medical care.
Screening for carriage of the HLA-B*5701 allele is recommended before re-administration of an abacavir-containing drug in patients with unknown HLA-B*5701 status who previously tolerated therapy with the containing drug.
Re-administration of an abacavir-containing drug to patients carrying the HLA-B * 5701 allele is not recommended and can only be considered in exceptional cases under close medical supervision, when the potential benefit of treatment with the drug outweighs all possible risks.
Lactic acidosis, hepatomegaly and fatty liver
When using antiretroviral nucleoside analogs (including abacavir and lamivudine), taken either alone or in combination, the development of lactic acidosis, hepatomegaly and severe fatty degeneration of the liver, including cases that ended in death, has been noted. Similar phenomena were observed mainly in women.
Clinical signs of developing lactic acidosis are: general weakness, anorexia, sudden unreasonable weight loss, symptoms of damage to the respiratory organs (shortness of breath, rapid breathing) and the gastrointestinal tract.
Caution should be exercised when prescribing the drug to all patients, especially those who have risk factors for liver damage. The drug should be discontinued if there are clinical or laboratory signs of lactic acidosis or hepatotoxicity (which include hepatomegaly and steatosis, even in the absence of a significant increase in the level of aminotransferases).
Lipodystrophy
Some patients treated with combination antiretroviral therapy have experienced redistribution/accumulation of body fat, increased fat on the back of the neck and back ("buffalo hump"), decreased peripheral fat, facial emaciation, breast enlargement, increased glucose levels and serum lipid levels.
Lipodystrophy can develop when taking any drugs from the class of protease inhibitors or nucleoside reverse transcriptase inhibitors. However, available data suggest that the risk of developing these side effects when taking different drugs of these classes is not the same.
In addition, many factors contribute to the development of lipodystrophy. An important and possibly mutually potentiating role is played by the presence of HIV infection, advanced age, and the duration of antiretroviral therapy.
During the clinical examination, attention should be paid to signs of redistribution of body fat. Serum lipid levels and blood glucose levels should be closely monitored. If necessary, carry out appropriate treatment of disorders of fat metabolism.
Patients with concomitant viral hepatitis B
Clinical studies and post-marketing data on the use of lamivudine suggest that some patients with concomitant viral hepatitis B may experience clinical or laboratory evidence of hepatitis recurrence after discontinuation of lamivudine. Discontinuation of lamivudine may have more severe consequences in patients with decompensated liver disease. As a result, in patients with concomitant viral hepatitis B, when the drug is discontinued, liver function tests should be monitored and the level of hepatitis B virus replication should be regularly determined.
immune reconstitution syndrome
If HIV-infected patients with severe immunodeficiency have asymptomatic or oligosymptomatic opportunistic infections at the time of initiation of antiretroviral therapy, such therapy may lead to an increase in the symptoms of opportunistic infections or other serious consequences. These reactions usually occur within the first weeks or months of onset.
antiretroviral therapy. Typical examples are cytomegalovirus retinitis, generalized or focal infection caused by mycobacteria, and pneumonia caused by Pneumocystis jiroveci (P. carini). The appearance of any symptoms of inflammation requires immediate examination and, if necessary, treatment.Opportunistic infections
The use of the drug or other antiretroviral drugs does not exclude the possibility of developing opportunistic infections or other complications of HIV infection, so patients should remain under the supervision of a physician experienced in the treatment of these diseases.
Transmission
Modern antiretroviral therapy, including the drug, does not prevent the transmission of HIV through sexual contact or contact with infected blood. Be aware of the need to comply with appropriate security measures.
myocardial infarction
As a result of a prospective, observational, epidemiological study to study the incidence of myocardial infarction in patients receiving combination antiretroviral therapy, an association was found with a previous 6-month intake of abacavir with an increased risk of myocardial infarction. According to a pooled analysis of clinical studies, there was no increase in the risk of myocardial infarction associated with taking abacavir. Biological mechanisms explaining the potentially increased risk are unknown. In general, available data from observational cohorts and controlled clinical trials do not unambiguously determine the association of abacavir therapy with the risk of myocardial infarction.
However, antiretroviral therapy, including preparations containing antiretroviral therapy, should be prescribed with caution to patients with a possible risk of coronary heart disease. All measures must be taken to minimize risk factors (such as arterial hypertension, dyslipidemia, diabetes mellitus and smoking).
Instructions Dosage form: film-coated tablets Composition:Composition per 1 tablet
Active ingredients: abacavir sulfate 702.6 mg (equivalent to 600 mg abacavir), lamivudine 300 mg.
Excipients: lactose monohydrate 40 mg, microcrystalline cellulose 44.4 mg, sodium carboxymethyl starch 7 mg, povidone-K 30 10 mg, talc 3 mg, magnesium stearate 3 mg.
The composition of the shell: povidone-K 30 1.5 mg, hypromellose 5 mg, talc 2 mg, titanium dioxide 1.44 mg, dye "sunset" yellow (E110) 0.06 mg.
Description:Tablets are capsule-shaped, biconvex, film-coated, yellow. On the cross section - the core is from white to almost white.
Pharmacotherapeutic group:Antiviral (HIV) agent ATX:J.05.A.R.02 Abacavir + Lamivudine
Pharmacodynamics:In all patients receiving therapy with the drug, the clinical diagnosis of suspected HSR should remain the basis for making a clinical decision.
If HSR is suspected, drug therapy should be stopped immediately, even in the absence of an allele.
HLA-B*5701. Delay in discontinuing drug therapy after the onset of HSR may result in a life-threatening reaction.Patients who develop HSR should be informed about the need to transfer the remaining tablets of the drug to the attending physician in order to avoid resuming abacavir.
Resumption of use of drugs containing after a suspected HSR on may lead to a rapid return of symptoms within a few hours, which may include life-threatening hypotension and death.
When considering resuming abacavir therapy after
discontinuation of treatment with any containing drug for any reason, the reason for discontinuation of therapy must be established, regardless of the carriage of the allele by the patient HLA -B*5701. If HSR cannot be excluded, the use of the drug or any other medicinal products containing .- If HSR is excluded, it is possible to resume drug therapy. In rare cases, patients who discontinued abacavir for reasons other than HSR symptoms have also experienced life-threatening reactions within a few hours of restarting abacavir therapy (see Description of Selected Adverse Reactions). Patients should be informed of the possibility of developing HSR when therapy is resumed with a drug or other medicinal products containing , and that the resumption of therapy with a drug or other medicinal products containing , should be carried out only if there is prompt access to medical care.
Clinical picture of HSR on abacavir
HSRs have not been well studied in clinical trials and during post-marketing surveillance. Symptoms usually appear within the first weeks (median time of onset of this reaction is 11 days) after the start of abacavir therapy, however, these reactions can develop at any time during therapy.
Virtually all HSR reactions do not include fever and/or rash as part of the syndrome. Other signs and symptoms that are noted as a manifestation of HSR on include respiratory and gastrointestinal symptoms, which can lead to misdiagnosis of HSR as a respiratory disease (pneumonia, bronchitis, pharyngitis) or gastroenteritis (see sections "Side effect ", "Description of individual adverse reactions"). With continued treatment, the severity of symptoms associated with HSR increases, and they can become life-threatening. In most cases, these symptoms disappear when you stop taking abacavir.
Lactic acidosis and severe hepatomegaly with steatosis
There are reports of the development of lactic acidosis, severe hepatomegaly with steatosis, including fatal, due to
APT nucleoside analogues in the form of individual drugs, including, or combinations thereof. Similar phenomena were observed mainly in women.Clinical signs of developing lactic acidosis include gastrointestinal symptoms (nausea, vomiting, and abdominal pain), general weakness, anorexia, loss of appetite, rapid unexplained weight loss, gastrointestinal and respiratory symptoms (shortness of breath and tachypnea), or neurological symptoms (including motor weakness).
Caution should be exercised when prescribing the drug, especially in patients with hepatomegaly, hepatitis or other risk factors for liver damage and hepatic steatosis (including certain drugs and alcohol).
Patients co-infected with hepatitis C and patients treated with alpha-interferon and ribavirin may be at particular risk. The use of the drug should be discontinued if there are clinical or laboratory signs of lactic acidosis with or without hepatitis (which include hepatomegaly and steatosis, even in the absence of a significant increase in aminotransferase activity), in conditions of symptomatic hyperlactatemia and metabolic acidosis / lactic acidosis, progressive hepatomegaly, or with a rapid increase in aminotransferase activities .
Lipodystrophy
Some patients receiving combined
APT, there may be a redistribution and / or accumulation of subcutaneous fat, including obesity but the central type, dorsocervical fat deposition ("buffalo hump"), a decrease in the subcutaneous fat layer on the face and extremities, an increase in the mammary glands, an increase in serum lipids and glucose concentrations in the blood, both individually and together.Although all drugs in the PI and NRTI classes can cause one or more of the adverse reactions listed above associated with a common syndrome often referred to as lipodystrophy, accumulating evidence suggests that there are differences between individual members of these drug classes in the ability to cause these adverse reactions.
It should also be noted that lipodystrophy syndrome has a multifactorial etiology: for example, stage of HIV infection, advanced age, and duration
APT play an important, possibly synergistic role in the development of this complication.The long-term effects of these adverse events are not yet known.
During a clinical examination, attention should be paid to signs of redistribution of subcutaneous fat. Need to be closely monitored
serum lipid concentration and blood glucose concentration. In violation of lipid metabolism, appropriate treatment is prescribed.Immune Restoration Syndrome
If HIV-infected patients with severe immunodeficiency have asymptomatic opportunistic infections or their residual effects at the time of initiation of ART, such therapy may lead to an increase in the symptoms of opportunistic infections or other serious consequences. These reactions usually occur within the first weeks or months of onset.
APT. Typical examples are cytomegalovirus retinitis, generalized or focal infection caused by mycobacteria, and pneumonia caused byPneumocystis jiroveci (R.carini). The appearance of any symptoms of inflammation requires immediate examination and, if necessary, treatment.Autoimmune diseases (such as Graves' disease, polymyositis, and Guillain-Barré syndrome) have also been observed during immune reconstitution, but the timing of onset varied and the disease could occur many months after initiation of therapy and have an atypical course.
Opportunistic infections
The use of the drug or other antiretroviral drugs does not exclude the possibility of developing opportunistic infections or other complications of HIV infection, so patients should remain under the supervision of a physician experienced in the treatment of these HIV-associated diseases.
HIV transmission
Patients should be warned that treatment with antiretroviral drugs, including the drug, does not prevent the risk of transmitting HIV to others through sexual intercourse or blood contamination. Therefore, patients should take appropriate precautions.
myocardial infarction
As a result of a prospective observational epidemiological study to study the incidence of myocardial infarction in patients receiving combined
APT, an association was found between previous use of abacavir within 6 months with an increased risk of developing myocardial infarction. According to a pooled analysis of clinical studies, there was no increase in the risk of myocardial infarction associated with taking abacavir. Biological mechanisms explaining the potentially increased risk are unknown. In general, the available data from observational cohorts and controlled clinical trials do notallow to unequivocally determine the relationship of abacavir therapy with the risk of myocardial infarction.However, caution should be given to
APT, including preparations containing, patients with a possible risk of coronary heart disease. All measures should be taken to minimize risk factors (such as arterial hypertension, hyperlipidemia, diabetes mellitus and smoking).Pancreatitis
Cases of pancreatitis have been reported, although a causal relationship between lamivudine and abacavir has not been clearly established.
kidney disease
The drug should not be administered to patients with creatinine clearance less than 50 ml/min.
Liver disease
The efficacy and safety of the drug has not been established in patients with severe concomitant liver disease. The drug is not recommended for patients with impaired liver function.
In patients with pre-existing hepatic impairment, including active chronic hepatitis, there is an increased incidence of hepatic impairment with combined
APT. Such patients should be monitored in accordance with standard clinical practice.Patients with chronic hepatitis B or C
Clinical studies and post-marketing surveillance data on the use of lamivudine suggest that in some patients with concomitant viral hepatitis B
(HBV) there may be clinical or laboratory signs of hepatitis recurrence after discontinuation of lamivudine, which may be more severe in patients with decompensated liver disease. As a result, in patients with concomitant viral hepatitis B, when the drug is discontinued, liver function tests should be monitored and markers of hepatitis B virus replication should be regularly determined.Due to the fact that and have the same phosphorylation pathways, an interaction between these substances is suggested, which can lead to a decrease in intracellular phosphorylation of ribavirin metabolites and potentially leads to a decrease in the likelihood of achieving a sustained virological response in hepatitis C co-infected HIV-infected patients treated with pegylated interferon and ribavirin.
Conflicting data have been published on the simultaneous use of abacavir and ribavirin. Some data suggest that HIV-infected patients receiving abacavir-containing drugs may be at risk of a low response rate to antiviral therapy with pegylated interferon and ribavirin. Care must be taken when taking these drugs at the same time.
Mitochondrial dysfunction
Research in vitro And in vivoshowed that nucleoside and nucleotide analogs can cause varying degrees of damage to mitochondria. Cases of mitochondrial dysfunction have been reported in HIV-negative children treated in utero and/or postnatally with nucleoside analogues. The main adverse reactions were hematological disorders (anemia, neutropenia), metabolic disorders (hyperlactatemia, hyperlipasemia). These adverse reactions are often transient. Some late-onset neurological disorders (increased muscle tone, seizures, behavioral disturbances) have been reported. Whether these neurological disorders are transient or permanent is currently unknown. Any child, even HIV-negative, exposed in utero to nucleoside and nucleotide analogues should undergo clinical and laboratory evaluation to rule out mitochondrial dysfunction if signs or symptoms are identified. These data do not affect current national recommendations for use. APT in pregnant women to prevent vertical transmission of HIV infection.
osteonecrosis
Although the etiology of this disease is multifactorial (including glucocorticosteroids, alcohol use, severe immunosuppression, high body mass index), cases of osteonecrosis most often occurred in patients with advanced HIV infection and/or long-term use of combined
APT. Patients should see a doctor if they experience joint pain and stiffness or difficulty moving.Risk of virological failure
Triple nucleoside therapy: A high rate of early virological failure and resistance has been reported when abacavir and lamivudine were co-administered with tenofovir disoproxil fumarate in a once daily dosing regimen.
contains sunset yellow dye which may cause allergic reactions. Influence on the ability to drive transport. cf. and fur.:No specific studies have been conducted on the effect of lamivudine on the ability to drive or use machines. In addition, a negative impact on such activities cannot be predicted based on the pharmacology of these drugs. When assessing the patient's ability to drive vehicles or mechanisms, his general condition should be taken into account, as well as the profile of adverse drug reactions.
Release form / dosage:Film-coated tablets, 600 mg + 300 mg. Package:On 10 tablets in the blister from aluminum foil and PVC of a film of amber color. On 1, 3 or 10 blisters together with the application instruction in a cardboard pack.
100, 500 or 1000 tablets in a plastic bag. 1 bag per HDPE-silica gel jar, sealed with PE-coated aluminum foil, with screw cap. A label made of label paper or writing paper or polymeric materials, self-adhesive, is glued onto the jar. 1.6, 12 or 24 cans, together with an equal number of instructions for use, are placed in a group package - a corrugated cardboard box (for hospitals).
Storage conditions:At a temperature not higher than 25 °C.
Best before date: 2 years. Do not use after the expiry date stated on the packaging. Conditions for dispensing from pharmacies: On prescription Registration number: LP-004209 Date of registration: 21.03.2017 Expiration date: 21.03.2022 Registration certificate holder: India Manufacturer: Representation: Lock-Beta Pharmaceuticals (I) Pvt.Ltd Information update date: 25.04.2017 Illustrated InstructionsINN: Abacavir, Lamivudine
Manufacturer: Aurobindo Pharma Limited
Anatomical-therapeutic-chemical classification: Lamivudine and abacavir
Registration number in the Republic of Kazakhstan: No. RK-LS-5 No. 020716
Registration period: 23.07.2014 - 23.07.2019
KNF (drug is included in the Kazakhstan National Formulary of Medicines)
ALO (Included in the Free Outpatient Drug Supply List)
ED (Included in the List of drugs in the framework of the guaranteed volume of medical care, subject to purchase from a single distributor)
Limit purchase price in the Republic of Kazakhstan: 988.75 KZT
Instruction
Tradename
Abacavir and lamivudine
International non-proprietary name
Dosage form
Film-coated tablets, 600 mg/300 mg
Composition
One tablet contains
active substances- abacavir sulfate 702.78 mg (equivalent to abacavir 600.00 mg), lamivudine 300 mg,
excipients: microcrystalline cellulose (Ceolus KG-802), sodium starch glycolate (type A), purified water, magnesium stearate,
shell composition: Opadry shell YS-1-13065-A Orange: hydroxypropyl methylcellulose 2910/hypromellose 6 cP, hydroxypropyl methylcellulose 2910/hypromellose 3 cP, titanium dioxide (E 171), macrogol/PEG 400, FD&C Yellow #6/Sunset Yellow FCF Aluminum Lacquer ( 5% - 18%) (E 110), Polysorbate 80, FD&C Yellow #6/Sunset Yellow FCF Aluminum Lacquer (38% - 42%) (E 110).
Description
Orange, modified capsule-shaped, film-coated tablets, debossed with "H" on one side and "27" on the other side.
Pharmacotherapeutic group
Antiviral drugs for systemic use. Antiviral drugs for the treatment of HIV infection, combinations. Lamivudine and abacavir.
ATX code J05AR02
Pharmacological properties
Pharmacokinetics
Absorption
After oral administration, abacavir and lamivudine are rapidly and well absorbed. In adults, the absolute bioavailability of abacavir and lamivudine is 83% and 80-85%, respectively. The maximum concentration in blood serum is observed after 1.5 hours and 1.0 hours, respectively. After a single oral administration of 600 mg of abacavir, the Cmax value is 4.26 µg/ml (28%), and the AUC∞ value is 11.95 µg h/ml (21%). After repeated oral administration of 300 mg lamivudine for 7 days, the Cmax value is 2.04 μg/ml (26%) and the AUC∞ value is 8.87 μg h/ml (21%). Eating does not significantly affect the effect of the drug, so Abacavir and lamivudine can be taken regardless of food intake.
Distribution
The mean apparent volume of distribution is 0.8 and 1.3 L/kg, respectively. Abacavir at therapeutic concentrations is slightly or moderately (about 49%) bound to human plasma proteins. Lamivudine exhibits linear pharmacokinetics over the therapeutic concentration range and low plasma protein binding (less than 36%), indicating a low potential for drug interactions. Abacavir and lamivudine penetrate the central nervous system and cerebrospinal fluid. The ratio of AUC in cerebrospinal fluid and blood plasma is 30-44%. Peak concentrations observed are 9 times greater than the IC50 of abacavir (0.08 μg/mL or 0.26 μmol) when abacavir is administered at 600 mg twice daily. The average ratio of lamivudine concentration in cerebrospinal fluid/serum within 2-4 hours after taking the drug is about 12%.
Metabolism
Metabolism of abacavir occurs predominantly in the liver. About 2% of the dose taken is excreted in the urine unchanged. The metabolism of abacavir in the human body is associated with the action of alcohol dehydrogenase and the formation of glucuronide conjugates - 5'-carboxylic acid and 5'-glucuronide. Their amount is about 66% of the dose taken and is excreted in the urine. Lamivudine undergoes negligible hepatic metabolism (5-10%) and is excreted in the urine mainly unchanged.
Elimination
The elimination half-life of abacavir is 1.5 hours. After repeated oral administration of the drug at a dose of 300 mg 2 times a day, no significant accumulation of the drug is observed. Excretion of abacavir occurs through hepatic metabolism, followed by excretion of metabolites in the urine. About 83% of the dose taken is excreted in the urine as metabolites and unchanged drug, the rest is excreted in the faeces. The elimination half-life of lamivudine is 5-7 hours. The mean total clearance of lamivudine is approximately 0.32 L/h/kg, which is predominantly renal clearance (over 70%) via the organic cation transport system.
Patients with impaired liver function
Abacavir is metabolized primarily by the liver. In patients with mild hepatic impairment (5-6 points on the Child-Pugh scale), abacavir AUC was increased by an average of 1.89 times, and the elimination half-life by 1.58 times. A slight impairment of liver function did not affect the AUC of abacavir metabolites, but the rate of formation and elimination of metabolites was reduced.
In patients with mild hepatic impairment data are not available. The pharmacokinetics of abacavir has not been studied in patients with moderate to severe hepatic impairment. It is expected that in such patients the concentration of abacavir in plasma will be variable and, in most cases, increased, and therefore the drug is contraindicated in this category of patients.
Moderate to severe liver disease does not significantly affect the pharmacokinetics of lamivudine.
Patients with impaired renal function
The pharmacokinetic parameters of abacavir in patients with end-stage renal disease and in patients with normal renal function are the same.
Due to reduced clearance in patients with renal dysfunction, the concentration-time ratio (AUC) of lamivudine is increased. Due to the need for dose reduction, patients with creatinine clearance less than 50 ml/min should be treated with lamivudine alone.
Pharmacodynamics
Abacavir and lamivudine is a combination drug that contains abacavir and lamivudine and has an antiviral effect.
Abacavir and lamivudine belong to the group of nucleoside reverse transcriptase inhibitors of HIV-1 and HIV-2. Abacavir and lamivudine are sequentially metabolized by intracellular kinases to the corresponding active forms of the drug - triphosphates (TF). Lamivudine triphosphate and carbovir triphosphate (the active form of abacavir triphosphate) are substrates and competitive inhibitors of HIV reverse transcriptase. Their main antiviral action is the conversion of monophosphate forms into the viral DNA chain, leading to subsequent chain termination. The triphosphates of abacavir and lamivudine show little resemblance to host cell DNA polymerases.
Lamivudine in combination with zidovudine shows synergy and suppresses the replication of the human immunodeficiency virus (HIV) in cell culture.
Abacavir shows synergism in combination with amprenavir, nevirapine and zidovudine and has an additive effect in combination with didanosine, zalcitabine, stavudine, lamivudine.
HIV-1 resistance to lamivudine involves the development of changes in the amino acid M184V close to the active site of the viral reverse transcriptase. M184V mutations reduce susceptibility to lamivudine. Viral strains resistant to zidovudine, while acquiring resistance to lamivudine, may become sensitive to zidovudine. The development of abacavir resistance is associated with specific genotypic changes in a specific codon region of reverse transcriptase (codons M184V, K65R, L74V and Y115F). Viral resistance to abacavir develops relatively slowly, multiple mutations are needed to increase the IC50 concentration by 8 times compared to the "wild" strain of the virus, which may be clinically significant. In strains resistant to abacavir, sensitivity to lamivudine, zalcitabine, tenofovir, emtricitabine and / or didanosine may be reduced, but sensitivity to zidovudine and stavudine remains. Cross-resistance is unlikely to develop between abacavir or lamivudine and other classes of antiretroviral drugs, such as protease inhibitors or non-nucleoside reverse transcriptase inhibitors.
Decreased susceptibility to abacavir has been demonstrated in clinically isolated strains in patients with uncontrolled viral replication who have previously received treatment and are resistant to other nucleoside inhibitors. Clinically isolated strains with three or more mutations associated with nucleoside reverse transcriptase inhibitors are unlikely to be susceptible to abacavir.
Cross-resistance inherent in M184V RT is limited within the nucleoside inhibitor class of antiretrovirals. Zidovudine, stavudine, abacavir, and tenofovir retain their antiretroviral activity against lamivudine-resistant HIV-1 containing only the M184V mutation.
Indications for use
HIV infection as part of combination antiretroviral therapy in adults
Dosage and administration
Abacavir and lamivudine should be prescribed by specialists with experience in the treatment of HIV infection.
Adults weighing over 40 kg Abacavir and lamivudine can be taken with or without food. The maximum daily dose is 1 tablet (600 mg / 300 mg) 1 time per day, daily.
Elderly patients
The pharmacokinetics of abacavir and lamivudine have not been studied in patients over 65 years of age. In the treatment of elderly patients, the increased incidence of liver, kidney, heart and other concomitant diseases, as well as the use of other drugs, should be taken into account.
Patients suffering from renal insufficiency
Patients suffering from liver failure
In patients with mild hepatic impairment (Child-Pugh A), a dose reduction of abacavir may be required. Since the reduction of individual components in the composition of the drug is not possible, it is necessary to prescribe abacavir and lamivudine preparations separately. The appointment of this drug in patients with moderate or severe hepatic insufficiency (Child-Pugh B and C) is contraindicated.
Side effects
This drug contains two active ingredients - abacavir and lamivudine, and below are the side reactions that may occur with their use. It is not clear whether these reactions are related to the drug, concomitant therapy, or are the result of a general disease.
Frequency of occurrence: very often (> 1/10), often (> 1/100,<1/10), нечасто (>1/1,000, <1/100), редко (>1/10,000, <1/1000), очень редко (<1/10,000).
Many of the following reactions are common (nausea, vomiting, diarrhea, fever, drowsiness, rash) and may indicate a hypersensitivity reaction. Thus, if any of these symptoms occur, the patient should carefully analyze these reactions for their relationship with the hypersensitivity reaction. If the drug was discontinued due to the development of any of the listed symptoms, but it was later decided to resume therapy, the use of Abacavir and lamivudine should be carried out under strict medical supervision.
Reactions to abacavir
Often
Hypersensitivity reactions
Anorexia
Headache
Nausea, vomiting, diarrhea
Fever, drowsiness, fatigue
Reactions to lamivudine
Often
Headache
Nausea, vomiting, upper abdominal pain, diarrhea
Weakness, fatigue, fever
Infrequently
Transient increase in liver enzymes (AST, ALT)
Anemia, neutropenia, thrombocytopenia
Post marketing data
Reactions to abacavir
Often
Hyperlactatemia
Rash (no systemic manifestations)
Seldom
Pancreatitis, but association with abacavir has not been established
Very rarely
Erythema multiforme, Stevens-Johnson syndrome, toxic epidermal necrolysis
Reactions to lamivudine
Often
Hyperlactatemia
Alopecia
Arthralgia, muscle disorders
Seldom
Lactic acidosis (redistribution/accumulation of fat has been identified in patients taking antiretroviral therapy. This pathology has a multifactorial etiology, including the combined use of antiretroviral drugs)
Increased serum amylase levels, pancreatitis, although the relationship with lamivudine has not been established
Rhabdomyolysis
Very rarely
Peripheral neuropathy, paresthesia, although no relationship has been established with lamivudine
Hypersensitivity reactions to abacavir
In clinical studies, during the screening process, approximately 5% of the subjects were found to have the HLA B * 5701 allele, which was associated with a significant risk of developing hypersensitivity reactions to abacavir, in rare cases with a fatal outcome. These reactions are manifested by symptoms that indicate multiple organ damage. In most cases, one of the manifestations of the hypersensitivity reaction was fever or rash (maculopapular or urticaria), however, hypersensitivity reactions can be observed in the absence of these symptoms.
Symptoms of hypersensitivity may appear at any time while taking abacavir, but more often this happens during the first 6 weeks of therapy (on average, on day 11 of therapy). The signs and symptoms of this hypersensitivity reaction are listed below. Those signs that occurred at least in 10% of patients, highlighted in bold:
- rash(usually maculopapular or urticarial)
manifestations of the oral mucosa, abdominal pain, nausea, vomiting, diarrhea
- shortness of breath, cough, sore throat, respiratory failure, respiratory distress syndrome
- fever, fatigue, malaise, edema, lymphadenopathy, hypotension, conjunctivitis, anaphylaxis
- headache, paresthesia
Lymphopenia
- increase in liver function tests, liver failure
Increased creatinine levels, renal failure
- myalgia, myolysis, arthralgia, increased levels of creatine phosphokinase
In some cases, hypersensitivity reactions can be interpreted as diseases of the respiratory system (pneumonia, bronchitis, pharyngitis), influenza-like illness, gastroenteritis, or reactions to other drugs. Delay in the diagnosis of hypersensitivity reactions may lead to continued use of abacavir and, consequently, to the development of more severe hypersensitivity reactions during administration. Thus, when hypersensitivity reactions are suspected, even in cases where the possibility of another diagnosis cannot be excluded, all listed symptoms should be carefully considered for a possible relationship with a hypersensitivity reaction. If a hypersensitivity reaction cannot be ruled out, the drug and other abacavir-containing products should be discontinued and should never be given in the future.
Symptoms associated with a hypersensitivity reaction worsen with continued therapy, and usually disappear after discontinuation of abacavir and other abacavir-containing drugs.
The resumption of abacavir in the presence of hypersensitivity reactions leads to the return of symptoms within a few hours.
Symptoms that develop with continued use of abacavir and lamivudine can be much more severe than symptoms that appear on the background of the first dose of the drug, and can lead to the development of life-threatening hypotension and death.
Regardless ofHLAB*5701 Patient status If any symptoms of hypersensitivity develop, the drug should be discontinued immediately. In the event of a hypersensitivity reaction, abacavir and lamivudine and any other abacavir-containing products should never be administered subsequently.
Several cases of hypersensitivity reactions have been identified when abacavir is restarted after its withdrawal due to the development of any one symptom of hypersensitivity (rash, fever, malaise/fatigue, gastrointestinal or respiratory symptoms).
In rare cases, hypersensitivity reactions may develop when abacavir therapy is resumed in the absence of previous signs and symptoms of hypersensitivity development.
Contraindications
Hypersensitivity to abacavir, lamivudine or any of the components of the drug
Moderate and severe liver failure
Renal failure with creatinine clearance less than 50 ml/min
Pregnancy and lactation
Children and adolescents up to 18 years of age
Drug Interactions
Since this medicinal product contains abacavir and lamivudine, any interactions that have been identified with these agents individually may occur. Abacavir and lamivudine are not significantly metabolized by cytochrome P450 enzymes (such as CYP 3A4, CYP 2C9 or CYP 2D6) and do not inhibit or induce this enzyme system. Therefore, the drug is unlikely to interact with antiretroviral protease inhibitors, non-nucleosides and other drugs that are metabolized by the main P450 enzymes.
The likelihood of interactions involving lamivudine is extremely low due to its limited metabolism and low plasma protein binding and almost complete elimination via renal clearance. Care must be taken when concomitantly prescribing those drugs that are also excreted by the renal mechanism.
Abacavir interactions
With ethanol
The metabolism of abacavir is impaired when used together with ethanol, which is accompanied by an increase in AUC by 41% and has no clinical significance. Abacavir does not affect the metabolism of ethanol.
With methadone
With the simultaneous use of abacavir at a dose of 600 mg 2 times a day day and methadone Cmax of abacavir decreased by 35%, and Tmax increased by 1 hour, the AUC indicator did not change. These data are of no clinical significance. Abacavir increases the systemic clearance of methadone by 22%, so a second dose adjustment of methadone may sometimes be required.
With retinoids
Retinoid Compounds excreted from the body by the enzyme alcohol dehydrogenase. Interactions with abacavir are possible but have not been studied.
Lamivudine interactions
With trimethoprim
Administration of trimethoprim/sulfamethoxazole 160 mg/800 mg (co-trimoxazole) resulted in a 40% increase in lamivudine exposure. If renal function is not impaired, then no dose adjustment of lamivudine is required. Lamivudine does not affect the pharmacokinetics of trimethoprim or sulfamethoxazole. The effect of lamivudine with high doses of co-trimoxazole in the treatment of pneumocystis pneumonia and toxoplasmosis has not been studied.
With zalcitabine
Lamivudine may inhibit intracellular phosphorylation of zalcitabine. The drug is not recommended for use with zalcitabine.
With emtricitabine
Lamivudine may inhibit intracellular phosphorylation of emtricitabine when these drugs are co-administered. Also, the mechanism for the development of viral resistance for both drugs occurs through mutation of the same regions of the viral transcriptase gene (M184V), respectively, the therapeutic efficacy of these products when used in combination may be limited. Lamivudine is not recommended for use with emtricitabine or products containing fixed doses of emtricitabine.
special instructions
Hypersensitivity to abacavir
In clinical studies, it was found that the presence of HLA B * 5701 in patients was associated with a significant risk of developing hypersensitivity reactions to abacavir (in 5% of the study), in rare cases leading to death.
Clinical studies have shown that carriage of the HLA B*5701 allele was associated with a significant increased risk of developing hypersensitivity reactions to abacavir. In studies where screening for the presence of the HLA B * 5701 allele in patients before treatment was used, the number of expected clinical hypersensitivity reactions to abacavir decreased from 7.8% (66 patients out of 847) to 3.4% (27 patients out of 803); and cases of hypersensitivity reactions confirmed by a skin test - from 2.7% (23 patients out of 842) to 0% (0 cases out of 802). Based on the study data, it was confirmed that 48-61% of patients with the HLA B*5701 allele carrier developed a hypersensitivity reaction while taking abacavir compared to those patients who did not have the HLA B*5701 allele (0-4%).
The attending physician should take into account the importance of screening for the presence of the HLA B * 5701 allele in patients before starting treatment with abacavir and lamivudine. Screening is also recommended before resuming the drug in patients with unknown HLA B * 5701 status who have previously received this drug and have shown tolerance to abacavir. When carrying the allele HLA B * 5701, the use of abacavir is not recommended; the appointment of abacavir-containing drugs is possible only under strict medical supervision and only if the potential benefit outweighs the possible risks.
It must be remembered that in patients using abacavir and lamivudine, any decision on the possibility of developing hypersensitivity reactions should remain dominant in the decision to prescribe the drug. Even in the absence of carriage of the HLA B * 5701 allele, it is important to remember the need to discontinue the drug if it is impossible to exclude the development of hypersensitivity reactions based on the available clinical data and not to prescribe abacavir-containing products in the future due to the potential for death.
Hypersensitivity reactions are manifested by symptoms that indicate multiple organ lesions. In most cases, one of the manifestations of the hypersensitivity syndrome was fever or rash, however, hypersensitivity reactions may be accompanied by other symptoms (fatigue, malaise, gastrointestinal symptoms such as nausea, vomiting, diarrhea, abdominal pain; respiratory symptoms such as dyspnea , sore throat, cough, infiltrates in the chest area).
Hypersensitivity reactions may develop at any stage of treatment with abacavir and lamivudine., but usually appear within the first 6 weeks from the start of the drug. With the withdrawal of the drug, the symptoms of hypersensitivity, as a rule, passed. With continued treatment, the symptoms worsen, which can threaten the patient's life.
Regardless ofHLAB*5701 status, the patient with the development of any symptoms of hypersensitivity should immediately report this to the attending physician. If the diagnosis of a hypersensitivity reaction is confirmed, Abacavir and lamivudine should be discontinued immediately. In the event of a hypersensitivity reaction, abacavir and lamivudine and any other abacavir-containing products should never be administered subsequently, as the most severe symptoms, including life-threatening hypotension, recur within hours and may be fatal.
To avoid delay in diagnosis and reduce the risk of life-threatening reactions, this drug should be discontinued if a hypersensitivity reaction is suspected, even if another diagnosis (eg, respiratory disease, influenza-like illness, gastroenteritis, or reactions) cannot be ruled out. for other drugs).
Taking the drug and other abacavir-containing products should not be resumed if hypersensitivity symptoms recur when alternative therapy is prescribed.
Regardless of the carriage of the HLA B * 5701 allele, if therapy with Abacavir and lamivudine has been suspended and a decision is made to continue it, it is necessary to carefully analyze the reasons for discontinuing the drug in order to exclude the possibility of symptoms of a hypersensitivity reaction. If hypersensitivity reactions cannot be ruled out, the drug or other abacavir-containing products should not be restarted.
In cases where a decision has been made to resume therapy in patients who have temporarily discontinued abacavir and lamivudine, it should be carried out in an appropriate medical institution and the patient should be able to receive urgent medical attention.
In some cases, hypersensitivity reactions may develop when abacavir therapy is resumed in the absence of previous signs and symptoms of hypersensitivity development. If a decision is made to resume therapy, the drug should be taken only if it is possible to provide immediate assistance to the patient.
Screening for HLA B*5701 carriage is recommended in patients of unknown status who are tolerant of prior abacavir treatment. When carrying the allele HLA B * 5701, the use of abacavir is not recommended; the appointment of abacavir-containing drugs is possible only under strict medical supervision and only if the potential benefit outweighs all possible risks.
When prescribing the drug, the doctor must be sure that the patient is informed of the following data on hypersensitivity reactions:
The patient should be aware of possible hypersensitivity reactions to abacavir and lamivudine, which may present with life-threatening or fatal symptoms, and of the increased risk of developing hypersensitivity reactions in the case of carriage of the HLA B*5701 allele.
The patient should be aware that even in the absence of the HLA B * 5701 allele, hypersensitivity reactions to this drug may develop. If the patient has symptoms that may be associated with a hypersensitivity reaction, he should contact his doctor immediately
Patients with hypersensitivity to abacavir and lamivudine should be aware that they should never again take it or any other drug containing abacavir despite HLA B*5701 status
In order to avoid self-resumption of therapy with Abacavir and lamivudine after the development of hypersensitivity reactions, the patient should return the remaining tablets to the doctor
Patients who stop taking the drug for any reason should consult a doctor before resuming the drug.
Lactic acidosis/severe hepatomegaly with steatosis
In HIV-infected patients (mainly women) who took antiretroviral drugs from the group of nucleoside analogues as monotherapy or as part of complex therapy, cases of lactic acidosis and hepatomegaly with fatty degeneration of the liver (including those with a fatal outcome) are described.
Clinical features that indicate the development of lactic acidosis include general weakness, anorexia and sudden unexplained weight loss, gastrointestinal and respiratory symptoms (shortness of breath and rapid breathing).
Caution should be exercised when treating with abacavir and lamivudine, especially if patients have risk factors for liver disease. In the event of clinical or laboratory signs of lactic acidosis with or without signs of hepatitis (which may include hepatomegaly and steatosis, even in the absence of an increase in transaminase levels), the drug should be discontinued.
Lipodystrophy
Some patients treated with combination antiretroviral therapy have experienced a redistribution/accumulation of body fat, including generalized obesity, dorsocervical obesity (buffalo hump), decreased peripheral fat, facial emaciation, breast enlargement, elevated serum glucose and lipid levels .
Side effects related to lipodystrophy may occur with any drug of the protease inhibitor or nucleoside reverse transcriptase inhibitor classes. However, available data suggest that the risk of developing these side effects when taking different drugs of these classes is not the same.
In addition, many factors contribute to the development of lipodystrophy. An important and possibly mutually potentiating role is played by the presence of HIV infection, advanced age, and the duration of antiretroviral therapy.
The long-term consequences of these violations are currently unknown.
During the clinical examination, attention should be paid to signs of redistribution of body fat. Serum lipid levels and blood glucose levels should be closely monitored. If necessary, carry out appropriate treatment of disorders of fat metabolism.
immune recovery syndrome
In severely immunocompromised HIV-infected patients on initiation of antiretroviral therapy (ART), an inflammatory response to asymptomatic or residual opportunistic infections may cause worsening of clinical symptoms of comorbidities. Usually, cytomegalovirus rhinitis, generalized and/or focal mycobacterial infections, and pneumocystis pneumonia were observed during the first few weeks or months after starting ART. Any inflammatory symptoms should be detected in a timely manner and, if necessary, appropriate anti-inflammatory therapy should be administered. Autoimmune disorders (polymyositis, Julian-Barr syndrome, diffuse toxic goiter) have also occurred while taking Abacavir and lamivudine, however, the time of disease attacks is quite variable and can occur many months after the start of therapy.
Patients with concomitant viral hepatitis B
In some patients with with concomitant viral hepatitis B (HBV), there may be clinical or laboratory signs of hepatitis recurrence after discontinuation of lamivudine, which, in turn, in patients with decompensated liver disease, may lead to more severe consequences. If abacavir and lamivudine were discontinued in patients with with concomitant viral hepatitis B, liver function tests should be monitored and levels of HBV replication markers should be measured regularly.
Opportunistic infections
Patients using abacavir and lamivudine or other antiretroviral drugs may develop infections caused by opportunistic microorganisms and other complications of HIV infection, so patients should be under the constant supervision of physicians experienced in the treatment of HIV infection.
Transmission
Patients should be informed that current antiretroviral therapy, including this drug, does not prevent the transmission of HIV to others through sexual intercourse or infected blood transfusion. Be aware of the need to comply with appropriate security measures.
Cardiovascular diseases
In studies aimed at determining the incidence of myocardial infarction in patients on combination antretroviral therapy, the use of abacavir for 6 months correlated with an increased risk of myocardial infarction. An analysis of clinical studies did not confirm an increase in the risk of myocardial infarction while taking abacavir. The biological mechanism for the potential increase in myocardial infarction is unknown. Thus, the relationship between abacavir and increased incidence of myocardial infarction remains unclear.
When prescribing antiretroviral therapy, including the drug Abacavir and lamivudine, to prevent the development of coronary heart disease, precautions should be taken to reduce all risk factors, such as hypertension, hyperlipidemia, diabetes mellitus, and smoking.
Features of the influence of the drug on the ability to drive a vehicle or potentially dangerous mechanisms
Special studies of the effect of lamivudine and abacavir on the ability to concentrate while driving vehicles / mechanisms have not been conducted. It is unlikely that the drug will adversely affect the ability to perform tasks that require concentration, motor or cognitive skills. However, when assessing the patient's ability to concentrate, their general condition should be taken into account, as well as the nature of the side effects that may occur while taking the drug Abacavir and lamivudine.
Overdose
Symptoms: increased side effects.
Treatment: in case of an overdose, the patient should be under the supervision of a physician (in order to identify signs of the toxic effect of the drug). If necessary, carry out standard maintenance therapy. Due to the fact that lamivudine can be removed from the body by dialysis, treatment of overdose should include continuous hemodialysis. It is currently unknown whether peritoneal dialysis and hemodialysis contribute to the elimination of abacavir from the body.
Release form and packaging
The active substance in the composition of the drug is a whole complex of compounds, which includes lamivudine, abacavir and zidovudine. Trizivir refers to the pharmacological group of combinatorial antiviral agents. It is used in the treatment of HIV infection in both adults and children.
Trizivir
Mechanism of action
All three active ingredients that make up Trizivir have the ability to block a specific viral enzyme called reverse transcriptase. This drug plays an important role in the reproduction of viral particles. Suppression of its activity stops the process of HIV DNA replicationApplication protocol
Trizivir is available in tablet form for oral administration. The standard dosage of the drug is 1 tablet, administered to the patient's body 2 times a day, regardless of the meal time.Usage efficiency
In clinical trials with Trizivir, it was shown that lamivudine, abacavir and zidovudine have the ability to significantly enhance the pharmacological action of each other. In the presence of all three compounds, the suppression of the replication of viral particles occurs much more intensively. In addition, the researchers specifically noted the low chemical affinity of the drug components for the DNA enzymes of ordinary human cells.Contraindications:
- allergic reactions to lamivudine, zidovudine or abacavir, as well as any other components that make up Trizivir;
- insufficiency of hepatic function;
- neutropenia;
- hemoglobin deficiency;
- the patient's age is less than 12 years.
Side effects of Trizivir:
- cardiomyopathy;
- anemic conditions, neutro-, leuko- and thrombocytopenia;
- nausea, sometimes vomiting;
- bowel disorder;
- pain in the stomach;
- loss of appetite and body weight;
- changes in the color of the oral mucosa;
- increased gas production in the intestines;
- pancreatitis;
- an increase in the size of the liver;
- joint and muscle pain;
- headaches and dizziness;
- sleep disturbances in the form of insomnia or, conversely, drowsiness;
- sensitivity disorders;
- convulsive syndrome;
- anxiety and depression;
- cough and shortness of breath;
- rash, itching and pigmentation of the skin;
- hives;
- hair loss;
- increased sweating;
- fever with chills;
- increasing weakness and fatigue;
- increased urination,
- gynecomastia.
Interaction with other drugs
Trizivir should be used under close medical supervision in conjunction with pharmacological agents such as:
- methadone;
- retinoid compounds;
- trimethoprim;
- zalcitabine;
- phenytoin;
- substances that block tubular secretion;
- ribavirin;
- rifampicin;
- stavudine.
 Basic Techniques for Cropping a Photo in Photoshop How to Uncrop a Photo in Photoshop
Basic Techniques for Cropping a Photo in Photoshop How to Uncrop a Photo in Photoshop Which acrylic brushes are better to choose: little secrets of choosing the right one Using different piles
Which acrylic brushes are better to choose: little secrets of choosing the right one Using different piles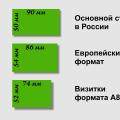 What are the sizes of business cards?
What are the sizes of business cards?